This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
The vater bulb, also known as the large papilla, is located in the middle part of the 2nd segment (D2) of the duodenum. Balloon stenosis is characterized by inflammation and fibrosis of the duodenal papillary muscle. But this definition still does not clinically describe the presence of recurrent abdominal pain after cholecystectomy.
The major duodenal papilla (different from the accessory duodenal papilla or the accessory pancreatic papilla) with the sphincter of Oddi is a complex structure in the human body. They secrete fluid under the stimulation of nerve factors, due to their anatomical location and complex structure, it will cause many disorders for the biliary tract and pancreas that Raskin discovered in 1985. The physiology and pathophysiology of the sphincter of Oddi is unclear despite numerous studies including the presence of endoscopic retrograde cholangiopancreatography. Since endoscopic sphincterotomy became possible, a method has changed or eliminated the function of the sphincter.
1. Clinical case
50-year-old female patient, non-laparoscopic cholecystectomy, common bile duct exploration. Six years later, the patient suffered from upper abdominal pain and jaundice secondary to cholangitis. These pains became more frequent and subsequently the patient was diagnosed with acute pancreatitis. The evaluation at this point included a transvenous cholangiogram showing a non-enlarged common bile duct, no stones, and a normal pancreatic duct. The catheter cannot be inserted into the common bile duct by endoscopic retrograde cholangiopancreatography and biliary papillary stenosis is suspected. The surgical findings included a wide bile duct without stones and a pressure-controlled cholangiogram showing no stained fluid entering the duodenum at 14, 20, and 30 cm of water. Flow through the biliary papilla at 30cm of water pressure was zero showing less pronounced than expected at 14cm of water.
After cholangioscopy, the smallest Fogarty catheter with 2 mm diameter cannot be passed through the papilla, as evidence of biliary papillary obstruction. Therefore, transduodenal biliary papillary reconstruction was performed. Under the microscope, pathology showed signs of chronic inflammation and biliary papillary fibrosis. Postoperatively, the patient was asymptomatic for 12 months. This case clearly showed biliary papillary stenosis and the presence of this disease was especially evident in symptomatic patients after cholecystectomy, who did not have common bile duct stones but had disease of the pancreas and who were treated with biliary papillary plastic surgery.
2. Narrow definition of ball vater (papules vater)
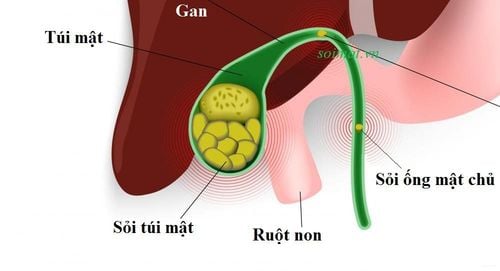
Before learning "what is vater ball narrowing", it is necessary to clearly understand "what is vater ball" and "where vater ball is located". The vater bulb, also known as the large duodenal papilla, is located in the middle part of the 2nd segment (D2) of the duodenum, where bile and pancreatic juice empties into the lumen of the duodenum to help digest food.
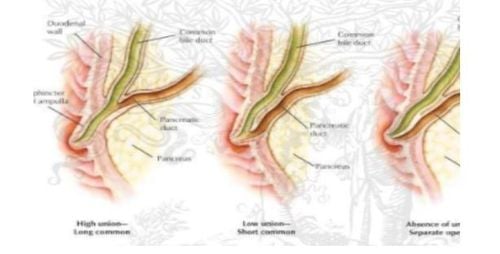
Cơ Vòng Oddi và sự hợp nhất của ống mật-tụy
3. Causes of narrowing of the ball of Vater
Papillary stenosis is thought to be the cause of pancreatitis and gallstones. However, pathological changes in the papillary muscle or dysfunction of the sphincter of Oddi do not necessarily cause biliary and pancreatic disorders. Choledocholithiasis is one of the clinical manifestations of papillary stenosis, however, the inextricable relationship between common bile duct stones and the sphincter of Oddi makes it difficult to determine the cause and influence the pathological changes. The mechanics of the sphincter of Oddi can lead to stone formation. The passage of small stones can cause narrowing of the papillary muscle. This etiology of biliary involvement may also apply to pancreatic pathology. Author Toouli et al studied abnormalities of the sphincter of Oddi in 25/28 patients with recurrent pancreatitis of unknown cause, but retrograde pancreatography also showed abnormalities in the majority of cases. The relationship between papillary stenosis and recognized disorders of the biliary system and pancreas has been studied by many authors.
The term papillary stenosis is associated with a clinical syndrome that includes biliary tract pain or acute pancreatitis. It is important to distinguish between symptoms of gallstones and recurrent pancreatitis, whereas patients with this syndrome have no evidence of bile duct stones or acute pancreatitis. Pathological changes may or may not be present in most sites of duodenal papillary stenosis but there is no evidence of stones in the liver, biliary tract, or pancreas.
Predisposing factors for biliary atresia include: Benign papillary stenosis - fibrosis or adenoma - obstructs the outflow of pancreatic bile and causes symptoms. The advantage to the persistence of biliary atresia may be evident. The etiology of biliary papillary stenosis is scarring at the site of injury secondary to gallstone removal or surgical manipulation or inflammatory infiltration from a nearby duodenal ulcer or acute superior papillary pancreatitis. The presence or absence of primary biliary papillary stenosis is controversial, although the finding of a history such as inflammation of the gland is probably the etiology. Primary or secondary biliary papillary stenosis cannot be clearly distinguished because the presence of gallstones can be considered as a secondary cause, thus factoring in and presence of gallstone disease with a single stone. Pure papillary traversal can never be ruled out.
4. Diagnosis of benign biliary papillary stenosis If symptoms occur in a patient who has had a cholecystectomy, the indication for another procedure today will depend on the results of endoscopic retrograde cholangiopancreatography. The inability to insert the probe into the papilla or the delayed exit of the bound dye from the common bile duct indicate papillary stenosis. When there is evidence of prevalence due to endoscopic biliary papillary dilation, these criteria are purely subjective and tend to be interpreted by individual background.
Objective data can be obtained by endoscopic exploration of the sphincter of Oddi, which has become an uncommon procedure due to its high cost. Therefore, there is no value on sphincter pressure for the treatment of biliary papillary stenosis. On the other hand, if biliary papillary stenosis is more frequent, symptoms are often attributed to gallstones. Therefore, biliary papillary stenosis must be resolved by surgery and surgical complications have a rate of 0-40%, so treatment is widely accepted.
Surgical examination includes:
Cholangiography. Measure the flow of bile. Bile papillae exploration. In summary, papillary stenosis is an imprecise term. Pathologically, sphincter stenosis is characterized by inflammation and fibrosis of the duodenal papillary muscle. But this definition still does not clinically describe the presence of recurrent abdominal pain after cholecystectomy.
References:
Le Quang Quoc Anh. The basics of sphincterotomy of Oddi and endoscopic gallstone removal. Gastrointestinal diseases. Ho Chi Minh City Digestive Science Conference 1998, 35 - 40. Le Quang Quoc Anh. Role of retrograde endoscopy in biliary-pancreatic pathology. Proceedings of the full text of scientific topics at the Vietnamese surgical conference. Surgical journal. Hue 2002, 61-70. David Fleischer. Endoscopic management of biliary tract obstruction. Techniques in therapeutic endoscopy. Saunders 1992.8.2-8.7. Franklin E. Kasmin, David Cohen, Subash Batra. Needle-knife sphincterotomy in a tertiary referral center: efficacy and complications. Gastrointestinal Endoscopy. Vol. 44, 1996, 48 - 53.






![[Video] Don't be subjective with gallstone disease](/static/uploads/small_20191104_030711_425223_soi_omc_max_1800x1800_jpg_2e7a54defa.jpg)





