This is an automatically translated article.
Autoimmune pancreatitis is one of the human autoimmune diseases. Autoimmune pancreatitis was only recently discovered (previously often confused with other conditions), a finding that now plays an important role in making treatment more effective.
1. What is autoimmune pancreatitis?
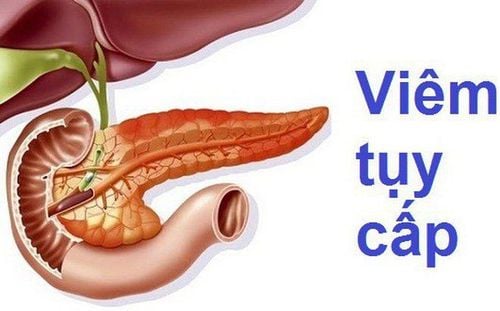
Autoimmune pancreatitis is a chronic inflammation caused by the body's own immune system attacking the body's own pancreas, limiting or not producing insulin, leading to diabetes; does not ensure the function of secreting digestive enzymes, leading to malnutrition or causing consequences such as eye damage, hypertension, foot ulcers...
Autoimmune pancreatitis is classified into two types as inflammation autoimmune pancreatitis type 1 and autoimmune pancreatitis type 2.
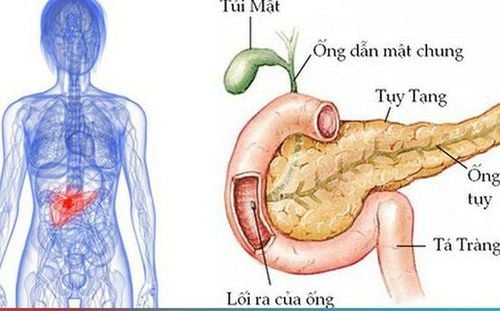
Autoimmune pancreatitis type 1 also known as IgG4-associated pancreatitis usually affects many organs including pancreas, intrahepatic bile ducts, salivary glands, kidneys and lymph nodes.
Autoimmune pancreatitis type 2, also known as idiopathic duct-centric pancreatitis, affects only the pancreas.
Autoimmune pancreatitis is a rare disease, until now the cause of the disease is still unknown, so correct diagnosis plays an important role in the treatment of the disease.
2. Risk factors for autoimmune pancreatitis
People with type 1 autoimmune pancreatitis are usually:
Over 60 years old. Is male. People with type 2 autoimmune pancreatitis:
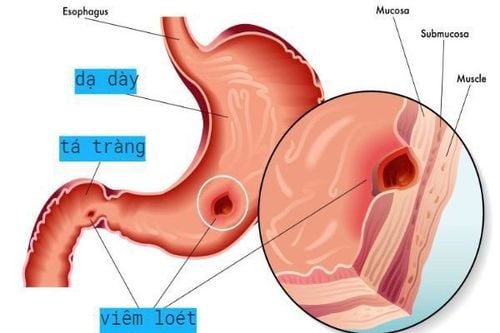
Usually over 40 years old (aged 10 to 20 years younger than people with type 1 autoimmune pancreatitis). The incidence is similar in men and women. Often have inflammatory bowel disease (such as ulcerative colitis). Autoimmune pancreatitis can cause a variety of complications:
Pancreatitis: Autoimmune pancreatitis affects the pancreas' ability to produce enzymes. Possible signs and symptoms include diarrhea, weight loss, metabolic bone disease, and vitamin and mineral deficiencies. Diabetes: The pancreas is the organ that produces insulin, so when the pancreas is damaged, it can cause diabetes. Pancreatic calcifications, pancreatic stones. Treatment for autoimmune pancreatitis (such as long-term steroid use) can also cause complications. However, despite complications, people treated for autoimmune pancreatitis still have a good quality of life.
Những người lướn tuổi có nguy cơ mắc viêm tụy tự miễn cao hơn
3.Symptoms of autoimmune pancreatitis
Autoimmune pancreatitis is quite difficult to diagnose. Usually autoimmune pancreatitis does not cause any symptoms, but if they do, they are similar to those of pancreatic cancer.
Symptoms of pancreatic cancer include:
Dark urine. Pale stools, or floating stools in the toilet. Yellow skin, yellow eyes. Upper abdominal or mid-back pain. Nausea, vomiting. Weak or extremely tired. Loss of appetite, feeling full. Unexplained weight loss. The most common sign of autoimmune pancreatitis is painless jaundice, caused by an obstructed biliary tree. Autoimmune pancreatitis can also cause weight loss. Many patients with autoimmune pancreatitis develop abnormal masses in the pancreas and other organs that are easily mistaken for cancer. Differences between type 1 autoimmune pancreatitis and other type 2 autoimmune pancreatitis include:
Autoimmune pancreatitis type 1 can affect organs other than the pancreas, whereas autoimmune pancreatitis type 2 only affects organs other than the pancreas. affects the pancreas, although type 2 autoimmune pancreatitis is associated with another autoimmune disease, colitis. Type 1 autoimmune pancreatitis responds rapidly to steroid therapy. Autoimmune pancreatitis type 1 is likely to recur after stopping treatment.
4. When to see a doctor
Autoimmune pancreatitis usually doesn't cause any symptoms, but see your doctor if you notice unexplained weight loss, abdominal pain, jaundice, or other suspicious signs and symptoms.
5. Diagnosis of autoimmune pancreatitis
Autoimmune pancreatitis is often difficult to diagnose because the signs and symptoms are easily confused with pancreatic cancer. However, getting the right diagnosis is important because the two diseases have different treatments.
Patients with autoimmune pancreatitis often have an enlarged pancreas, but an abnormal mass in the pancreas may also be present.
There is no single test that can identify autoimmune pancreatitis. Sometimes surgery is needed to rule out pancreatic cancer.
Tests may include:
Imaging: Computed tomography, magnetic resonance imaging, endoscopic ultrasound, endoscopic retrograde cholangiopancreatography. Blood tests: People with type 1 autoimmune pancreatitis often have elevated levels of IgG4 in their blood. Endoscopic core biopsy. Steroid trial: Because autoimmune pancreatitis is the only steroid-responsive pancreatic disease, this approach can be used to confirm the diagnosis.

Ngoài chụp cộng hưởng từ, viêm tụy tự miễn có thể được chẩn đoán bằng cách xét nghiệm máu
6. Treatment of autoimmune pancreatitis
Steroids: Autoimmune pancreatitis responds very well to steroids, some people even responding extremely quickly. Immunosuppressive drugs: About 30 - 50% of patients after treatment have a relapse of autoimmune pancreatitis, so to avoid the side effects caused by prolonged steroid treatment, the doctor may prescribe immunosuppressive drugs. Treatment of pancreatic insufficiency: Supplementing pancreatic enzymes with prescription drugs such as Creon, Pancreaze, Zenpep, Pertzye. Treatment of diabetes. Monitor other organs: Because type 1 autoimmune pancreatitis can affect many other organs. Chronic pancreatitis is a serious chronic disease on the gastrointestinal tract, affecting the patient's health. Due to the function of the pancreas, so far it has not been able to completely reconstruct it by artificial means. However, having knowledge to prevent this disease, detect and actively treat it right from the beginning will partly reduce the severe effects that the disease causes.
If you have unusual symptoms, you should be examined and consulted with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Articles refer to the source: mayoclinic.org