This is an automatically translated article.
It is estimated that approximately 20% to 40% of patients with atrial fibrillation have concomitant coronary artery disease (CAD), a sizable proportion of whom require revascularization with percutaneous coronary intervention (PCI). ) and stenting. Such patients require dual antiplatelet therapy (DAPT) to prevent the risk of stent thrombosis and additional thrombotic ischemic events. Read more to understand more about anticoagulation in atrial fibrillation after percutaneous coronary intervention.
1. Why should anticoagulation in AF after percutaneous coronary intervention?
Atrial fibrillation (AF) is a common condition in the elderly. Atrial fibrillation increases the risk of thromboembolic complications, including stroke and extracranial systemic embolic events, which require prophylaxis with oral anticoagulation (OAC). Overall, approximately 5% to 10% of patients presenting for coronary angiography with or without percutaneous coronary intervention present with atrial fibrillation or other indications.
The optimal antithrombotic regimen for patients with atrial fibrillation undergoing percutaneous coronary intervention is a clinical conundrum. Theoretically, a combination of oral anticoagulants and dual antiplatelet therapy, a regimen also known as triple antithrombotic therapy (TAT), is required to reduce both the risk of thromboembolism and thromboembolism. atrial fibrillation and the risk of coronary stent thrombosis events in patients with underlying coronary artery disease. However, antithrombotic drugs increase the risk of heavy bleeding in patients, which can even lead to death. There are already several randomized controlled trials comparing antithrombotic drugs with alternative antithrombotic regimens, such as dual antithrombotic therapy (DAT), in combination with oral anticoagulants. with single antiplatelet therapy (SAPT).
Patients with atrial fibrillation require oral anticoagulation to prevent the risk of thromboembolic events, whereas antiplatelet therapy is required to prevent stent thrombosis in the setting of percutaneous coronary interventions .
2. Percutaneous coronary intervention
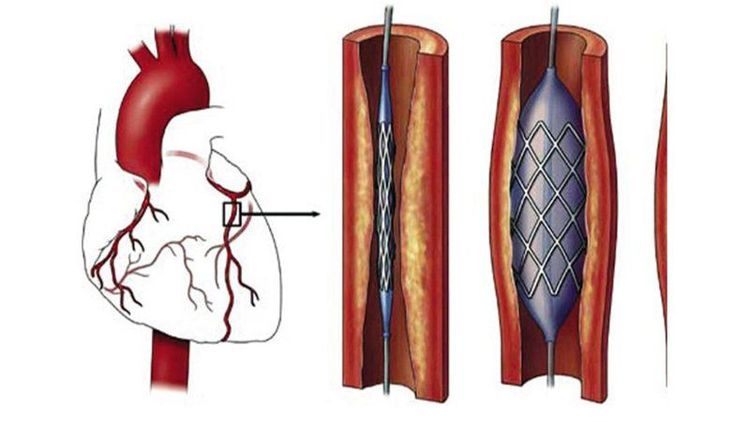
2.1. What is percutaneous coronary intervention? Percutaneous coronary intervention (PCI, formerly known as stent angioplasty) is a non-surgical procedure that uses a catheter (a thin, flexible tube) to place a small structure called a stent to open up blood vessels. Blood in the heart has been narrowed by plaque buildup, a condition known as atherosclerosis.
Why is it done?
Percutaneous coronary intervention improves blood flow, thereby reducing heart-related chest pain (angina), making you feel more comfortable and increasing your ability to function. Percutaneous coronary intervention is usually scheduled in advance.
Can thiệp mạch vành qua da giúp mở các mạch máu trong tim bị thu hẹp do mảng bám tích tụ
What is done?
A catheter is inserted into blood vessels in the groin or arm.
Using a special type of X-ray called fluoroscopy, a catheter is threaded through the blood vessels into the heart where the coronary arteries are narrowed.
When the balloon tip is in place, a balloon tip covered with a stent is inflated.
The ball head compresses plaques and dilates the stent.
Once the plaque is compressed and stented, the balloon is deflated and withdrawn.
The stent is in the artery, keeping it open.
What can you expect from percutaneous coronary intervention?
Your doctor will explain the risks and benefits of the procedure. Before the procedure begins, tell your doctor if you:
Have ever had a reaction to any contrast, iodine or any serious allergic reaction (for example, to a bee sting or to eat shellfish). Have asthma. Are allergic to any medications. Have bleeding problems or are taking blood thinners. Have a history of kidney problems or diabetes. Wear piercings on your chest or belly. Have any recent changes in your health. Are, or may be, pregnant. Shortly before the procedure, you may receive a sedative to help you relax. Hair may be trimmed in the groin area around the catheterization site.
An intravenous (IV) line is inserted so you can get medicine quickly if needed.
Electrodes will be placed on your body to monitor your heart and a small device called a pulse oximeter can be attached to your finger or ear to monitor the oxygen level in your blood.
Most percutaneous coronary interventions are performed with patients sedated but not asleep.
A local anesthetic will be injected into the skin at the site where the catheter will be inserted.
When it has worked, the catheter will be inserted into the blood vessel.
You may feel a stinging or brief sting as the needle goes through the skin and some pressure in the artery as the catheter is moved. If you feel discomfort, tell your doctor and, if necessary, give more pain medication.
When the catheter reaches the heart, contrast will be released so the area of the narrowed blood vessel can be identified.
As the dye is released, you may feel a slight flushing or warm feeling. Some people experience a salty or metallic taste in their mouth or a short-term headache. Some people may feel nauseous or even vomit, but this is rare. These effects are harmless and usually last only a few minutes.
When a narrowing is identified, the catheter will be raised to activate the special tip.
You may feel pain or discomfort in your chest at this point, but your doctor will monitor you carefully and the discomfort should go away quickly.
When finished, the catheter will be withdrawn and pressure is applied to the site to stop bleeding.
Once the bleeding has stopped, a tight bandage will be applied.
You will need to lie flat during this time.
If the catheter has been inserted into the groin, you will have to keep your leg straight for several hours.
If it is attached to the arm, your arm will be kept on the pillow and held straight by an arm board.
After the procedure
You will probably go to the recovery room for several hours of observation.
You will be asked to stay in bed for 2 to 6 hours, depending on your specific condition.
Pain medicine may be given if you feel discomfort.
You will be encouraged to drink water and other fluids to help clear the contrast from your body.
Most people spend the night in the hospital after percutaneous coronary intervention.
At home
When you return home, pay attention to the insertion position. A small bruise is normal, but contact your doctor if you experience:
Increased pain Redness Swelling Bleeding or other discharge from the insertion site Fever Chills.

Người bệnh được chăm sóc và theo dõi vị trí chèn sau khi can thiệp mạch vành qua da
2.1. Clinical Trials Over the past few years, research has focused on the treatment of patients with atrial fibrillation within the first 12 months of PCI. On the basis of these studies, current guidelines recommend triple therapy (oral anticoagulants plus aspirin and P2Y inhibitors) for as short a time as possible for immediate antithrombotic therapy. i.e. for patients with atrial fibrillation who have undergone percutaneous coronary intervention and whose ischemic risk outweighs the bleeding risk. Such treatment is followed by combination therapy with an oral anticoagulant plus a P2Y inhibitor for 4 to 6 weeks 8 or up to 12 months in selected patients. After 12 months of combination therapy, or in patients with AF and stable coronary artery disease who do not require intervention, current guidelines recommend oral anticoagulant monotherapy. However, this approach is not yet supported by evidence from randomized, controlled trials. Furthermore, a significant number of patients in this condition continue to receive combination therapy, which indicates a gap between guidelines and clinical practice.
A previous randomized, controlled trial that evaluated the efficacy and safety of oral anticoagulant monotherapy versus combination therapy with an oral anticoagulant plus an antiaggregation agent. Single platelet count in patients with atrial fibrillation and coronary artery disease stabilized more than 1 year after stenting, but this trial was ineffective and fruitless because enrollment was terminated early. In the AFIRE trial (Atrial fibrillation and ischemia with rivaroxaban in patients with stable coronary artery disease), we aimed to investigate whether monotherapy with rivaroxaban (a vitamin-free oral anticoagulant). K) is not inferior to the combination of rivaroxaban and antiplatelet agents in patients with atrial fibrillation and stable coronary disease more than 1 year after revascularization or in patients with confirmed coronary artery disease. The pathological aspect does not require recanalization.
A group of men and women aged 20 years and older were diagnosed with atrial fibrillation and stable coronary artery disease in Japan. During the screening process, the researchers rated the patients on CHADS2 on a scale of 0 to 6, with higher scores indicating a higher risk of stroke; Congestive heart failure, hypertension, diabetes and age 75 and older are scored 1 point, and previous stroke or transient ischemic attack are scored 2 points. Patients were required to have a score of at least 1 on the scale. Patients must also meet at least one of the following criteria: history of percutaneous coronary intervention, including angioplasty with or without stenting, at least 1 year prior to admission; history of coronary artery disease confirmed by angiography (with stenosis ≥50%) does not require revascularization; or history of coronary artery bypass graft (CABG) at least 1 year prior to admission. The primary exclusion criteria were a history of stent thrombosis, coexisting active tumor, and poorly controlled hypertension.
To further assess stroke risk, the researchers used the CHA2DS2 -VASc score, which is associated with improved stratification among low-risk patients. Patients were evaluated based on the five criteria of the CHADS2 scale plus three additional criteria: history of vascular disease, age 64 to 74, sex. The score is divided from 0 to 9, with the age of 75 and above being 2 points; Higher scores indicate greater risk. The researchers also assessed the risk of major bleeding on the HAS-BLED scale, which ranges from 0 to 9, with higher scores indicating a greater risk of bleeding.
Study randomized patients in a 1:1 ratio to rivaroxaban monotherapy (10 mg once daily for patients with creatinine clearance between 15 and 49 ml per minute or 15 mg per day). once for patients with creatinine clearance ≥50ml per minute) or combination therapy with rivaroxaban at the previously stated dose plus an antiplatelet agent (aspirin or P2Y 12 inhibitor - ticagrelor and clopidogrel, depending on decision of the treating physician).
Bác sĩ khuyến nghị nên kết hợp sử dụng thuốc để chống đông trong rung nhĩ sau can thiệp động mạch vành qua da
2.2. Considerations in PCI Until recently, warfarin therapy has been considered standard therapy for stroke prevention in patients with high-risk atrial fibrillation. According to the results of a meta-analysis performed by Lip et al and published in 2002, treatment with warfarin reduced 62% (95% CI 48% to 72%) stroke or systemic embolism compared with placebo. and 36% (95% CI 14% to 52%) reduction in stroke or systemic embolism compared with aspirin. Warfarin is also significantly more effective in preventing stroke than aspirin-clopidogrel combination therapy in patients with atrial fibrillation, which has been proven by research of many experts around the world.
After percutaneous coronary intervention, especially if accompanied by stenting, standard antithrombotic therapy is the aspirin-clopidogrel combination. In the clinical trials ISAR (Intra Coronary Stenting and Antithrombotic Regimen trial) and STARS (Stent Anticoagulation Regimen Study) performed in patients with coronary stents, aspirin plus ticlopidine (a thienopyridine analog with clopidogrel) was administered. many adverse events should not be circulating) significantly reduced major cardiovascular events (death, myocardial infarction, stent thrombosis, target coronary reperfusion) compared with aspirin alone and aspirin in combination with warfarin. 4.5
A major challenge for physicians is antithrombotic treatment of patients undergoing percutaneous coronary intervention with atrial fibrillation. Treatment must both prevent stroke and systemic embolism associated with atrial fibrillation and effectively prevent thrombosis causing coronary stent occlusion. The problem is that when all three drugs are combined (both warfarin, and aspirin-clopidogrel), the risk of bleeding increases dramatically. How to balance the effectiveness of thrombosis prevention on the one hand and minimize the risk of bleeding on the other hand is a very difficult task for the physician, especially when there are not many clinical data to allow the determination of an appropriate strategy. near optimal.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.