This is an automatically translated article.
Chronic pancreatitis is a persistent, untreated, chronic pancreatitis that results in permanent damage to pancreatic structures, fibrosis and duct compression, and impaired exocrine and endocrine function. . Heavy alcohol use and smoking are considered two major risk factors for chronic pancreatitis.
1. What is chronic pancreatitis?
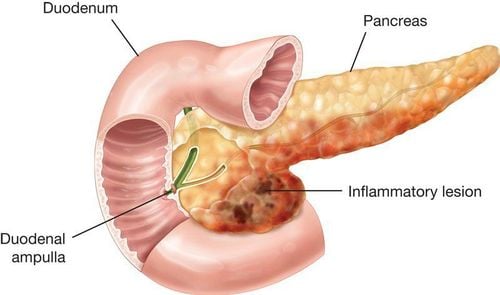
The pancreas is a long and flattened gland, located behind the stomach, in the upper abdomen (epigastric region) with 2 main tasks:
Producing digestive enzymes into the small intestine to help digest food; Production and release of the hormones insulin and glucagon into the bloodstream. These two hormones are responsible for regulating and stabilizing blood sugar. After prolonged episodes of acute pancreatitis, damage to the pancreatic parenchyma leads to chronic pancreatitis. This is a pathological process that causes irreversible pancreatic damage, fibrosis, and destruction of pancreatic tissue.
2. The link between heavy alcoholism and chronic pancreatitis
Chronic pancreatitis has fibrosis of the pancreatic parenchyma, the increasingly severe destruction will lead to the decline or loss of pancreatic function. Clinically, there are many causes leading to chronic pancreatitis, of which more than 70% of chronic pancreatitis is caused by alcohol abuse and heavy alcohol abuse.
Pancreatic damage due to alcoholism is often insidious, not manifesting for many years, then suddenly presented by an episode of acute pancreatitis. It can be seen that heavy alcoholism is the main cause of chronic pancreatitis in 70% of adults, more common in men than in women, and usually occurs between the ages of 30 and 40.
There are also other causes of chronic pancreatitis:
Obstruction, narrowing of the pancreatic duct due to trauma or the formation of pancreatic pseudocyst; Hereditary, unspecified (idiopathic); Metabolic disorders: protein deficiency, excess fat; Lead poisoning, mercury poisoning; Autoimmune causes; Caused by certain drugs; Pulmonary cystic fibrosis.

Nghiện rượu nặng được xem là yếu tố nguy cơ chính gây viêm tụy mạn tính
3. Symptoms of Chronic Pancreatitis
The majority of patients with chronic pancreatitis experience abdominal pain. However, there are still many patients without pain symptoms. The pain often becomes worse after the patient eats and drinks, the pain can spread to the back or the pain is continuous, sometimes even making the patient unable to function normally.
In some cases, the pain may decrease gradually as the disease progresses because the pancreas is no longer able to produce digestive enzymes. In addition, the patient may also have some other symptoms including: nausea, vomiting, weight loss, fatty diarrhea ...
Patients with chronic pancreatitis often lose weight even though they still feel good eating. mouth and is following a normal diet. This phenomenon of weight loss occurs because the patient's body is no longer able to secrete enough pancreatic enzymes to digest food, resulting in nutrients not being fully absorbed. Poor digestion also leads to the excretion of fat, protein and sugar in the stool.
4. Complications of chronic pancreatitis
When lipase and protease enzyme secretion falls to <10% of normal, the patient develops the malabsorption characteristic of chronic pancreatitis with lipolysis. Then the movement of the stool will feel greasy, or even have oil droplets floating in the water, which are difficult to clean with normal flushing.
In severe cases of chronic pancreatitis, malnutrition, weight loss, and malabsorption of fat-soluble vitamins (A, D, E, and K) may occur in the patient.
When insulin-producing cells in the pancreas (pancreatic islet beta cells) are also damaged in chronic pancreatitis, diabetes also develops. Thus, diabetes mellitus is a subsequent pathology, often occurring late in the progression of chronic pancreatitis.
Patients with chronic pancreatitis are also at risk for hypoglycemia. This is thought to be due to the destruction of the alpha cells of the pancreatic islet - the cells responsible for producing glucagon (the hormone that regulates the rise in blood sugar when blood sugar drops) has been destroyed.
Other complications of chronic pancreatitis:
Formation of pseudocysts; Obstruction of the bile duct or duodenum; Rupture of pancreatic duct (may cause ascites or pleural effusion); Thrombosis of the splenic vein, gastric vasodilation; Aneurysm near the pancreas or pseudocyst; Chronic pancreatitis increases the risk of pancreatic cancer, which is greatest in patients with hereditary pancreatitis and tropical pancreatitis. If chronic pancreatitis is left untreated, the disease will progress and develop complications within the first 10 years, most commonly malabsorption and diabetes.

Đa số bệnh nhân mắc bệnh viêm tụy mãn tính gặp phải tình trạng đau bụng
5. Chronic pancreatitis treatment
Diagnosis of chronic pancreatitis requires tests of pancreatic function: ultrasound technique, endoscopic retrograde cholangiopancreatography (ERCP), CAT scan... can show signs of chronic pancreatitis such as: : pancreatic calcification, hardening of pancreatic tissue due to precipitation of insoluble calcium salts...
When complications such as diabetes and malabsorption will occur, the doctor will order blood tests and tests to be performed. urinalysis, stool test to diagnose chronic pancreatitis and monitor complications of the disease.
Medical treatment in chronic pancreatitis is very important. Indications for surgery will be considered when the patient has persistent abdominal pain, unbearable pain and pain that has no longer responded to medical treatment with drugs. Surgery for chronic pancreatitis is done with drainage of the pancreatic duct (connecting the pancreatic duct to the intestine) or surgical removal of all or part of the pancreas in severe cases.
Specific treatment steps are as follows:
Pain relief: the first step in treatment; Establish a high-carbohydrate, low-fat diet; Use pancreatic enzymes if the patient's pancreas is no longer able to respond enough, pancreatic enzymes need to be taken with each meal to support food digestion and weight improvement. Insulin may be prescribed to control blood sugar; Surgical drainage of an enlarged pancreatic duct due to obstruction or surgical removal of a necrotic part of the pancreas. In addition, patients need to completely give up alcohol, strictly follow the diet and complete medication schedule as prescribed by the doctor. To effectively treat chronic pancreatitis, you should see a hospital as soon as possible.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.