This is an automatically translated article.
The article was written by doctors of Internal Oncology Department - Vinmec Times City International General Hospital.About 10-20% of breast cancers are triple negative breast cancers. Doctors as well as researchers are very interested in finding new drugs to treat triple negative breast cancer. Current studies are trying to understand that some drugs can interfere with the development of triple negative breast cancer.
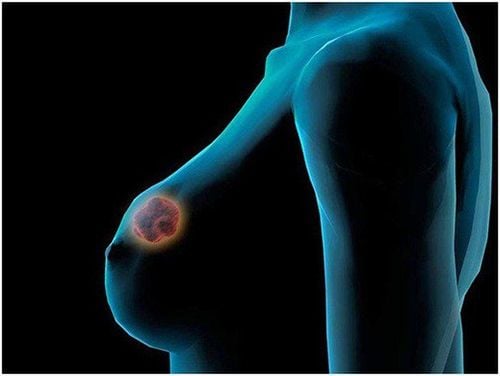
Triple negative breast cancer is a cancer that is estrogen, progesterone, and HER2 receptor negative.
This means that cancer growth is not driven by the hormones estrogen and progesterone, or by the HER2 protein. Therefore, triple negative breast cancer does not respond to hormone therapy drugs or drugs that target the HER2 protein receptor, but is successfully treated with other drugs.
1. What is triple negative breast cancer?
Cell receptors are special proteins on the inside and on the surface of cells. These receptor proteins are the "eyes and ears" of the cell, receiving messages from substances in the blood and telling the cell what to do.
Hormones attach to receptors and give instructions to help cells continue to grow and function. Not all breast cancer cells have hormone receptors. About two out of three breast cancers test positive for one or both of these hormone receptors.
About 20% of breast cancers make too much of the HER2 protein. In normal, healthy breast cells, HER2 stimulates cell growth. However, breast cancer cells with too much HER2 protein will grow and divide very quickly. Hormone therapies that disrupt the effects of estrogen, progesterone, and the HER2 protein on breast cancer can help slow or stop breast cancer cell growth.
About 10-20% of breast cancers are negative for both hormone receptor and HER2, meaning triple negative. When hormones do not promote cancer growth, the cancer will not respond to hormone treatment drugs, including tamoxifen and aromatase inhibitors. Triple-negative breast cancer also does not respond to drugs that target the HER2 protein, such as Herceptin (chemical name: trastuzumab), Kadcyla (chemical name: T-DMA or ado-trastuzumab emtansine), Nerlynx (chemical name: T-DMA or ado-trastuzumab emtansine). chemical name: neratinib), Perjeta (chemical name: pertuzumab) or Tykerb (chemical name: lapatinib).
2. Characteristics of triple negative breast cancer
Triple-negative breast cancer is considered malignant and has a poorer prognosis than other types of breast cancer, because there are few drugs to treat. Triple-negative breast cancer is more likely to metastasize outside the breast and recur after treatment. Triple-negative breast cancer usually has a higher grade than other types of breast cancer. The higher the grade, the less the cancer cells resemble normal healthy breast cells in shape and growth pattern. On a scale of 1 to 3, triple-negative breast cancer is usually grade 3. Triple-negative breast cancer often resembles a basal like , that is, like the basal cells that connect to the breast ducts. The basal like group tends to have a faster progression and more malignancy - like triple-negative breast cancer. Not all basal-like breast cancers are triple-negative breast cancers.
Trắc nghiệm: Những lầm tưởng và sự thật về ung thư vú
Ung thư vú có tỷ lệ tử vong cao nhất ở nữ giới khiến họ rất lo sợ bản thân mắc phải căn bệnh này. Tuy nhiên, không ít chị em có những hiểu biết thái quá về ung thư vú. Thử sức cùng bài trắc nghiệm sau sẽ giúp bạn loại bỏ được những nghi ngờ không đúng về căn bệnh này.
Bài dịch từ: webmd.com
3. Who is more likely to get triple negative breast cancer?
Anyone can get triple negative breast cancer. However, researchers have found that the disease is more common in the following populations:
Young people: Triple-negative breast cancer is more likely to be diagnosed in people younger than 50 years of age. Other types of breast cancer are usually diagnosed in people age 60 and older. African-American and Hispanic women: Triple-negative breast cancer is more likely to be diagnosed in African-American and Hispanic women. Asian women and non-Hispanic white women are less likely to be diagnosed with this type of cancer. People with BRCA1 mutations: About 70% of breast cancers are diagnosed in people with an inherited BRCA mutation, especially BRCA1, which is triple negative.

4. Treatment of triple negative breast cancer
This is a breast cancer that is more aggressive than other types and does not respond well to treatments that target the hormone receptor or the HER2 protein. However, lack of hormone receptors is only one factor that your doctor will consider when deciding on a treatment plan. The stage and malignancy of the cancer are also important for prognosis.
Triple-negative breast cancer is usually treated with a combination of surgery, radiation, and chemotherapy. Here are some treatments for this group of diseases:
4.1 Neoadjuvant chemotherapy
Research has shown that when triple negative breast cancer is treated with chemotherapy before surgery - called neoadjuvant chemotherapy - there is a complete pathological response, disease-free survival and overall better survival.
One way to assess the effectiveness of neoadjuvant treatment is to see if the tissues removed during surgery have any active cancer cells. If there are no active cancer cells, doctors call it a complete disease response, or pCR.
Disease-free survival is how long a person lives without the cancer coming back. Overall survival is how long a person lives whether or not the cancer comes back.

4.2 PARP . Inhibitors
PARP inhibitors, such as Lynparza (chemical name: olaparib) and Talzenna (chemical name: Talazoparib), have been approved for the treatment of advanced HER2-negative breast cancer with a BRCA1 or BRCA2 mutation.
The enzyme poly ADP-ribose polymerase (PARP) repairs DNA damage in both cancer and healthy cells. Research has shown that drugs that interfere with or inhibit the PARP enzyme also make it harder for cancer cells with BRCA1 or BRCA2 mutations to repair DNA damage. This makes it harder for cancer cells to survive. In other words, PARP inhibitors make some cancer cells less likely to survive damage to their DNA.
4.3 Immunotherapy
The immunotherapy drug Tecentriq (chemical name: atezolizumab) in combination with the chemotherapy drug Petexane (chemical name: albumin-bound paclitaxel or nab-paclitaxel) is approved as first-line cancer treatment. locally advanced inoperable triple negative breast or distant metastases, for which PD-L1 is positive.
Active immunotherapy drugs help the immune system work more effectively to attack cancer cells. Tecentriq is an immune checkpoint inhibitor, that is, it targets a specific protein that helps cancer cells hide from the immune system, in this case the protein PD-L1. By inhibiting PD-L1, Tecentriq allows immune system cells to see cancer cells.
Vinmec International General Hospital is currently providing a Breast Cancer Screening Package, which helps women detect breast cancer early even when there are no symptoms, thereby planning early treatment, increasing the survival prognosis for women. patient. Examination package with the following outstanding advantages:
Team of highly specialized and experienced doctors. Comprehensive professional cooperation with domestic and international hospitals in Singapore, Japan, USA, etc. Comprehensive treatment and care, multi-specialty coordination towards individualizing each patient. Having a full range of specialized facilities to diagnose the disease and stage it before treatment: Endoscopy, CT scan, PET-CT scan, MRI, histopathological diagnosis, gene-cell testing, .. There are a full range of mainstream cancer treatment methods: surgery, radiation therapy, chemotherapy, stem cell transplant...
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: Medscape












