This is an automatically translated article.
Acute myeloid leukemia (AML) is a malignancy of the bone marrow, involving platelets, erythrocytes, and erythrocytes. Acute leukemias are grouped in a variety of ways, with their own typical clinical signs and requirements for post-treatment care.1. Classification of acute myeloid leukemia by morphology
Acute myeloid leukemia was first described according to the morphology, characteristics of cancer cells when observed under the microscope. Diseases are classified according to the type of white blood cell that most closely resembles the diseased cells.The majority of AML patients belong to a group of diseases that primarily affect the production of neutrophils, called myeloblasts. Others belong to a group that involves abnormalities of monocytes, called monocytes. In addition, the pathology of acute leukemia has a combination of the two groups above.
Sometimes, AML also comes from the cells responsible for producing red blood cells, called erythrocytes, and the giant cells of the bone marrow that make platelets later. Acute promyelocytic leukemia (APL) is a special subtype of AML in which malignant cells stop maturing very early. APL is associated with translocation mutations between chromosomes 15 and 17.
According to the World Health Organization (WHO), acute myeloid leukemia is classified into the following main groups:
AML with abnormalities usually genes, which means variations on specific chromosomes. AML with polylinear dysplasia or abnormal blood cell morphology. AML associated with cell-damaging therapies is also known as treatment-associated myeloma. Unclassified AML Myeloma proliferation associated with Down syndrome. Pathologically indistinguishable leukemia. The FAB (French - American - British) classification is an older classification system that is still widely used today.
Acute myeloid leukemia M0: undifferentiated myeloblastic leukemia M1: poor or immature myeloblastic leukemia M2 : adult myeloblastic leukemia M3: pre-myeloblastic Leukemia M4: myeloblastic leukemia with monocytic Acute myeloid leukemia M4eo: myeloblastic with eosinophils Acute myeloid leukemia M5a: monocytic undifferentiated Acute myeloid leukemia M5b: differentiated monocytic Acute myeloid leukemia M6: associated with erythroblasts Acute myeloid leukemia M7: associated with giant nuclear cells.

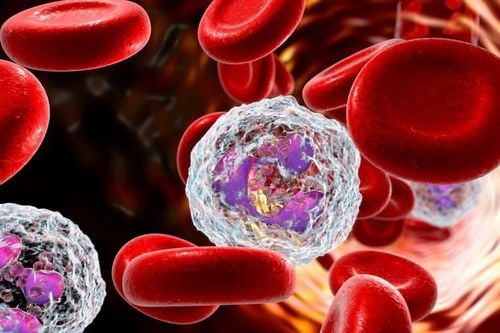
Hình ảnh bạch cầu cấp dòng tủy
2. Classification of acute myeloid leukemia according to cytogenetics
AML is also classified based on the cytogenetic, or chromosomal, changes found in pathological cells. Some chromosomal alterations are strongly associated with AML cell morphology. More importantly, chromosomal abnormalities help doctors find the best treatment because they can predict how well intensive treatments will work. Chromosomal alterations are usually grouped according to the likelihood that treatment will work for the AML subtype.The human genome has 23 sets of chromosomes, numbered 1 through 22, and 1 pair of X or Y sex chromosomes. Some of the types of specific genetic changes found in AML include :
Translocation Mutation Detachment Deleting Mutation. Some of the most common chromosomal changes are grouped as follows:
Advantage: chromosomal abnormalities have a higher chance of successful treatment, including translocations or inversions in the p13 and q22 bands of the chromosome 16 and translocations between chromosomes 8 and 21. Intermediate: changes associated with poor prognosis, including chromosomal normal, in which no changes are found, and translocations between chromosomes 9 and 11. Many other subtypes are considered part of this group, especially those with one or more changes at the molecular level. Occasionally, triploid mutations of chromosome 8 (trisomy 8) also fall into this category. Disadvantage: chromosomal changes associated with less successful treatment or low cure rate for AML include: aneuploidies of chromosomes 8 or 13, total or partial deletions number 5 or 7, multiple complex variations on multiple chromosomes and a change on chromosome 3 in the q26 band. Overall, the group of favorable changes was more common in younger patients, while adverse changes were more commonly seen in those over 60 years of age. Appropriate treatment varies between groups. Long-term treatment outcomes for 50% to 60% of patients under 60 years of age with AML are classified as favorable, and less than 10% of patients under 60 years of age with AML are classified as unfavorable. The prognosis in patients over 60 years of age is significantly worse. Choosing the right treatment depends on many other factors, including white blood cell counts. It is not possible to accurately predict the likelihood of successful treatment for a person with AML.

Một số các loại thay đổi di truyền đặc hiệu được tìm thấy trong bệnh AML
3. Classification of acute myeloid leukemia by molecular changes
Examining molecular changes in the diagnosis helps in the selection of a patient's treatment. For example, patients with NPM1 or CEBPalpha gene changes have a better distant prognosis, while chemotherapy does not work as well for patients with FLT3 gene changes. Other genetic alterations associated with prognosis for people with AML include:RUNX1 ASX11 P53 IDH1 and IDH2
4. AML recurrence
Recurrent AML is cancer that has come back after treatment. If the AML comes back, there will be another check to determine the extent of the recurrence. Tests are often similar to those performed at baseline. If you have unusual symptoms, you should be examined and consulted with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: cancer.netMORE:
What is leukemia? Common Types of Leukemia What is the number of white blood cells in the body?