This is an automatically translated article.
Article written by Doctor Le Van Quang - Ear, Nose Throat Doctor - General Surgery Department - Vinmec Nha Trang International General Hospital
In 1836, a German physician, Wilhelm Friedrich von Ludwig (1790-1865) in an unnamed editorial, published in two popular journals of the time, the Gazette Medicale de Paris and Schmidt's Jahrbucher, first described described a rapidly progressive infection of the soft tissues of the neck and floor of the mouth, which was almost fatal, due to airway obstruction, and was later named after Ludwig's edema (Ludwig's Angina).
Before antibiotics, this condition caused more than 50% mortality. Today, in the era of the development of antibiotics and the advancement of many diagnostic means in terms of imaging and intervention. This mortality rate has dropped impressively to about 8%.
1. Cause
The most common cause is infection of the lower molars, especially the second and third teeth, which account for more than 90% of cases. The infection begins in the subgingival pocket and directly extends rapidly to the musculature of the floor of the mouth, the sublingual space, under the chin, and the submandibular space.
Less common causes, including trauma to the floor of the mouth, fracture of the jaw, trauma to the tongue, piercing in the oral region, osteomyelitis, trauma from intubation, peritonsillar abscess, gland stones submandibular and glossopharyngeal cystitis.
Predisposing factors include diabetes, oral malignancy, dental caries, alcoholism, malnutrition and other immunocompromised conditions.
Infectious agents involving the oral microbiota, both aerobic and anaerobic. The most common are Staphylococcus, Streptococcus, Peptostreptococcus, Fusobacterium, Bacteroides and Actinomyces. Immunocompromised patients are at high risk of Ludwig edema.
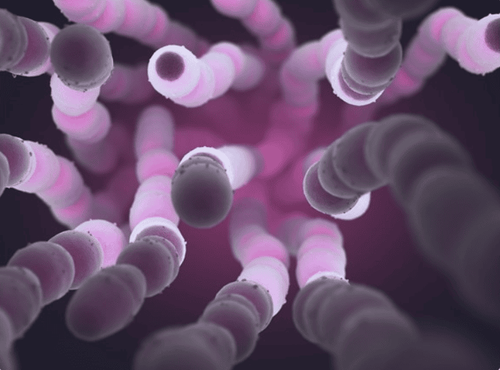
Hệ vi khuẩn miệng là một trong các tác nhân gây ra bệnh phù Ludwig
2. Symptoms and things to pay attention to when visiting
Swelling and pain in the neck, resembling “bull neck” Jaw stiffness or limited opening of the mouth High bulge tongue, dysarthria and dysphagia often due to sublingual effects Fever and chills Common Pain Pain mouth, hoarseness, drooling Sometimes a particularly rare pattern can be seen as a double tongue. Watch for stridor (Stridor), meaning airway obstruction is impending. Patients usually will not have lymphadenopathy. If there is a crackling sound to the touch, suspect other conditions, such as necrotizing fasciitis.
3. Diagnosis
Diagnosis is mainly based on clinical symptoms and disease history
The most important thing to remember is airway assessment, for prompt management
Tests are often of little value direct diagnosis. Blood cultures should be performed for sepsis.

Xét nghiệm thường ít có giá trị trong chẩn đoán bệnh trực tiếp
Imaging has no significant role in the immediate evaluation of the patient, but the decision to intubate should be weighed against all clinical parameters as soon as Ludwig's edema is diagnosed.
CT scan of the soft tissue neck with intravenous (IV) contrast can be used to assess the severity of the infection and assess for any abscesses, after the airway has been secured.
4. Treatment
Airway control is paramount in the treatment of Ludwig's edema, as the most common cause of death is sudden asphyxia due to airway obstruction.
Awake fibroptic intubation is an optimally safe way to secure an airway, and be prepared for emergency tracheostomy while awake at any time, before when performing any other intervention. Such as surveying the oral area to determine the source of infection. Drain the abscess in case it does form.
Usually bronchoscopy can be very difficult because of swelling of the oral cavity and bulging of the tongue.
It is important to manage the airways before presenting with dizziness or cyanosis as these are late findings.
If the patient cannot be intubated, the next step will be emergency tracheostomy.
Early broad-spectrum IV antibiotics are the first choice of treatment when the airway is secure and blood cultures have been obtained. For immunocompromised patients, a reasonable first choice would be ampicillin-sulbactam or clindamycin.

Người bệnh được dùng kết hợp kháng sinh khi đường thở được đảm bảo và đã cấy máu
Antibiotics should include against gram-positive, gram-negative and anaerobic bacteria.
For immunocompromised patients, range should be extended with pseudomonads.
Some options include cefepime, meropenem, or piperacillin-tazobactam.
IV steroids are controversial and are weighted based on the clinician's judgment on a case-by-case basis. Several recent reports suggest a benefit in reducing airway interference with steroid use. However, more research is needed before it becomes a standard of care.
The duration of antibiotics is usually two weeks with careful monitoring of the patient's response to medication. Extract the tooth if the source of infection is from the tooth.
For patients who do not respond to initial antibiotics or develop a collection of fluid, needle aspiration or surgical incision can be performed to drain, surgery in case of treatment failure, as early surgery does not proved to be more effective. Except for patients requiring intubation due to oral infection.
Differential diagnosis
Perimandibular abscess Posterior pharyngeal abscess Submandibular abscess Epiglottitis Oral carcinoma Angioedema Submandibular hematoma and diphtheria Although Ludwig's edema is a clinical diagnosis at first, it can be difficult to distinguish from other diseases. Imaging may be helpful to confirm the diagnosis and rule out other causes, but should ONLY be indicated after the airway is secured or in patients who are able to breathe comfortably and under control. secretions while lying on the back.

Chẩn đoán lâm sàng khó phân biệt phù Ludwig với các bệnh khác
Prognosis
Remember, one of the leading causes of death from Ludwig's edema is airway obstruction. The use of antibiotics and strict airway management should be implemented, and coordination in the role of prognostication and monitoring of progress between specialties such as otolaryngology, anesthesiology as well as nursing care should be taken. Follow-up care is essential, to be ready for possible interventions at any time. Mortality rate is estimated at 8%.
Currently, the Department of Dentistry - Jaw - Facial of Vinmec International General Hospital is a specialty in charge of intensive and aesthetic pathological treatment on the entire tooth structure (teeth, bone, pulp,... ), jaw (palatine, jawline, jaw joint,...) and face (frontal bone, cheekbone, temporal bone,...).
Dental - Jaw - Facial Department is divided into main specialties, in order to serve the needs of patients such as: Restorative dentistry, maxillofacial trauma, general dentistry, cosmetic dentistry and Interior.
Along with that, the Department of Dentistry - Jaw - Facial - Vinmec International General Hospital owns a team of reputable doctors with many years of experience in dental - jaw - facial problems such as: Doctor Hoang Mai Anh, Doctor Vu Duc Nha, Master. Doctor. Le Ngoc Tuan, Doctor Vu Hoang, Master. Doctor Lai Do Quyen.
To be examined by experienced Dental - Jaw - Facial specialists at Vinmec. Please make an appointment at the website to be served
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
See more:
Numbness in the first half, the left molar is a sign of what disease? How do teeth grow in the correct position? Is jaw pain after tooth extraction worrisome?







