This is an automatically translated article.
Full-thickness skin grafting is a method of removing skin patches on the body and grafting them onto areas of skin that are lost due to primary or secondary causes. Full-thickness skin grafting aims to provide a patch of skin for the area of skin loss to avoid the phenomenon of pulling that affects the aesthetics or the loss of skin is not able to close.1. What is a full-thickness skin graft?
Full thickness skin graft is a technique using a piece of skin, in which the patch of skin contains the entire epidermis and dermis, but no dermis, to graft into the area of skin loss. The thickness of a full-thickness skin graft is typically 0.8 to 1.5 mm, varying depending on the site of graft removal.Normally, a full-thickness skin graft contains a complete set of nerve endings, hair follicles, and excretory glands. Therefore, the full-thickness skin graft has better nerve redistribution from the wound background, more hair growth, more secretion from the sweat and sebaceous glands, but the secretion of the sweat glands is still dependent on the skin. neural redistribution of skin grafts.
Possible locations for skin grafts: Because the quality, color, texture and thickness of full-thickness skin pieces are different in each area of the body, usually the corresponding skin sites will be suitable to graft into the skin loss area with similar structure.
If the skin defects are in the face and neck area: The best place for the skin is the face and neck area, so it will ensure the similarity and the higher viability after transplantation of the skin in this area. Skin can be taken behind the ears, upper eyelids, upper clavicle. However, the disadvantage is that the graft in this region is limited in size. Some mobile skin areas can get more skin such as elbow folds, inguinal folds, inner thighs, lower abdomen, inner arms... Places where large skin grafts can be obtained such as: Buttock crease skin , inguinal folds, lower abdomen. The skin in this area can be directly closed to the donor site and the scar ensures better aesthetics after the skin graft is taken.
2. Indications and contraindications for full-thickness skin grafts
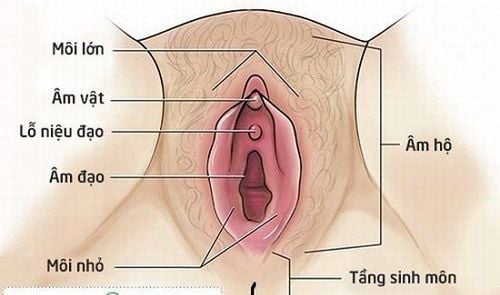
Indications for full-thickness skin graftCovering primary soft spot defects such as: New wounds have a good graft background, no exposed tendons, cartilage, joints or cases where periosteum, tendon membrane is still present. choroid... Wounds with skin defects that have formed granulomatous tissue Injuries caused by burns and have been removed with necrotic tissue Covering soft tissue defects due to secondary causes are formed such as: Conducting skin grafts after surgical removal of skin lesions such as scars formed after burns, melanoma, benign skin tumors, malignant skin tumors... After plastic surgery there are using local flaps, adjacent flaps, free flaps (The flap is a tissue that has nourishing blood vessels, ensuring it can be moved from a normal anatomical position to another location on the body). The flap donor site cannot be closed directly, requiring skin grafting. Shaping some organs and parts with three-dimensional structures such as: shaping urethra, vagina, eyelids, earlobes, nostrils, nipple areola unit... Preparing for a plastic surgery Covering other defects such as: Any soft tissue defects that are not yet eligible to conduct skin stretching techniques, then skin grafting to the base of the lesion is considered a necessary preparation step to avoid complications such as infection. for the next technique including natural skin stretching or skin stretching technique.

Ghép da dày toàn bộ được chỉ định trong trường hợp điều trị sẹo bỏng
Patients with blood clotting disorders, anemia, health is not guaranteed to perform skin grafting techniques. Do not transplant skin on the basis of receiving skin without good blood supply such as bones, tendons, cartilage, old granulomatous tissue. Do not graft skin on the background of the recipient is infected, skin lesions are necrotic. Do not graft skin on the background of malignant lesions On skin areas such as pressure ulcers or sacrum, radiation treatment areas, vasculitis, poor blood supply, areas with poor nutritional capacity, skin grafting should be considered. Consider skin grafting or limit skin grafting to areas that require high aesthetics such as the face or neck.
3. Steps to perform a full-thickness skin graft
3.1 Preparation before skin grafting The patient and family are explained in detail about the plan and the entire surgical procedure, the risks that may occur during and after surgery so that they can cooperate in the process. surgery. The night before surgery, the patient should have a light meal and take a bath, and use sedatives if he is too nervous and worried. Before surgery, the skin grafting area is cleaned with soap, Betadine, then the entire area is sterile gauze. In the area of skin defects, change the dressing, clean the wound and use a sterile gauze dressing... 3.2 Preparation of the receiving ground For a successful full-thickness skin graft, a good foundation must be prepared. Therefore, it is necessary to prepare the background:For wounds with primary soft tissue defects, it is necessary to assess the status of infection, conduct excision of necrotic tissues if present, evaluate the granulation and Perfusion status of the lesion background, it is necessary to determine the size of the lesion, evaluate the surrounding healthy skin... For the lesions with poor nutrition, it is necessary to regenerate the granulation tissue. Secondary skin defects need to determine the defect size, evaluate the blood supply status of the skin defect background. 3.3 Steps for full-thickness skin grafting Step 1: Prepare position The patient lies in a position to expose the receiving area.
Step 2: Conducting anesthesia Depending on the location, choose an appropriate anesthesia method such as general anesthesia or spinal anesthesia.
Step 3: Take the skin graft First choose the location and size of the skin grafting area to match the place where the graft is received.
The skin area is thoroughly disinfected with Betadine and alcohol 70 degrees.
Then conduct local anesthesia with 0.5% Lidocaine solution and 1:200,000 ratio of adrenaline if no general anesthesia.
Incision of the skin and separating the skin from the donor containing only the epidermis and dermis, removing all the fatty tissue of the remaining dermis.
After being removed, the skin graft must be immediately soaked in physiological saline, antibacterial agents such as antibiotics can be added.
Step 4: Carry out skin grafting Place the piece of skin taken on the grafting platform, stretch it moderately, then sew and attach the skin piece to the shore. After stitching, put a layer of gauze over it, put gauze on the tuber and a moderate pressure bandage. Leave the graft site immobilized for 7 to 10 days.

Người bệnh sẽ được giải thích quy trình ghép da dày toàn bộ trước khi phẫu thuật
4. Follow-up after total skin graft surgery
It is necessary to monitor complications and promptly handle possible complications. Shock, shock: Can occur immediately and after injection of anesthesia, this condition may be caused by the drug or by the patient's anxiety. Treat according to the anti-shock regimen, encourage and explain to the patient if the patient is overly worried. The skin piece does not adhere to the underlying tissue, necrosis of the graft: Usually due to inflammation, poor physical condition, the patient has a high blood sugar index, the graft foundation is not well prepared or when fixed. poor grafting region. Treatment: Change the bandage daily to check and correct the cause. Use systemic antibiotics, anti-inflammatory, pain relievers. Change the dressing of the graft after about 48 hours, regularly check the condition of the skin graft for color, nutrition, stagnant fluid, infection... Change the dressing area every other day with sterile gauze. If the patient has high blood sugar, it is necessary to have good control of blood sugar and need to actively treat accompanying diseases. In order for the full-thickness skin grafting technique to be convenient, it is necessary to have a good assessment of the receiving background, and to perform it by an experienced surgeon. Therefore, skin grafts should be performed at reputable addresses.Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: healthvietnam.vn