Management of progression of chronic kidney disease in patients with nonalcoholic fatty liver disease
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Doctors recommend that patients with diabetes and non-alcoholic fatty liver disease regularly monitor for underlying renal dysfunction, rather than just patients with diabetes. Monitoring of thyrotropin and thyroid hormone levels may be of clinical benefit when assessing the risk of developing chronic kidney disease in patients with nonalcoholic fatty liver disease; however, future studies are needed to specifically address the risk of CKD in patients with NAFLD and hypothyroidism.
1. Body weight
Waist-to-hip ratio: Few studies have evaluated the impact of weight loss on the progression of chronic kidney disease in patients with NAFLD. Recent studies have shown that reducing the waist-to-hip ratio (WHR) in patients with nonalcoholic fatty liver disease reduces the risk of developing chronic kidney disease. Serial WHR monitoring may be beneficial in identifying patients with NAFLD at risk for CKD. One limitation of this finding is that the reduction in WHR did not differentiate between reductions in visceral and subcutaneous fat. Studies have shown that visceral fat, but not subcutaneous fat, is a major contributor to the pathogenesis of nonalcoholic fatty liver disease through increased insulin resistance. However, with regard to a reduced risk of chronic kidney disease, the implications of reducing visceral and subcutaneous fat have not been well studied.
Weight loss: Data from the post hoc analysis of a clinical trial of 261 patients with nonalcoholic fatty liver disease showed a statistically significant relationship between body weight loss and eGFR changes ( when accounted for by the collaboration of chronic kidney disease -Epidemiology and dietary modification in the renal disease equation), even after adjusting for drug, diabetes, and hypertension profiles. In addition, patients with improved liver histology due to lifestyle changes such as weight loss were associated with significantly improved renal outcomes. Overall, patients with NAFLD who lost more than 5% of their weight and/or lost more than 5% of their WHR had improved renal outcomes.
Sodium-glucose cotransporter type-2 inhibitors: In patients with type 2 diabetes, sodium-glucose cotransporter type-2 inhibitors (SG liver transplant 2) have an established role in improving glycemic control , weight loss, cardiovascular outcomes, and decreased serum uric acid levels. In patients with type 2 diabetes, the landmark CREDENCE trial found that patients treated with a liver transplant SG inhibitor 2 (i.e. canagliflozin) had improved outcomes related to chronic kidney disease. Furthermore, recent evidence has shown that liver transplantation SG inhibitors 2 can also ameliorate TE-determined progressive NAFLD and biomarkers in NAFLD. alcohol (ie, liver enzymes). As liver transplant SG inhibitor 2 reduces serum uric acid levels, this may also contribute to the positive effects of this type on both diseases. In addition to facilitating glucoseuria, liver transplant SG-2 inhibitors are thought to reduce inflammation and reactive oxygen species formation, which are key in the pathogenesis of fatty liver disease. non-alcoholic and non-alcoholic steatohepatitis.

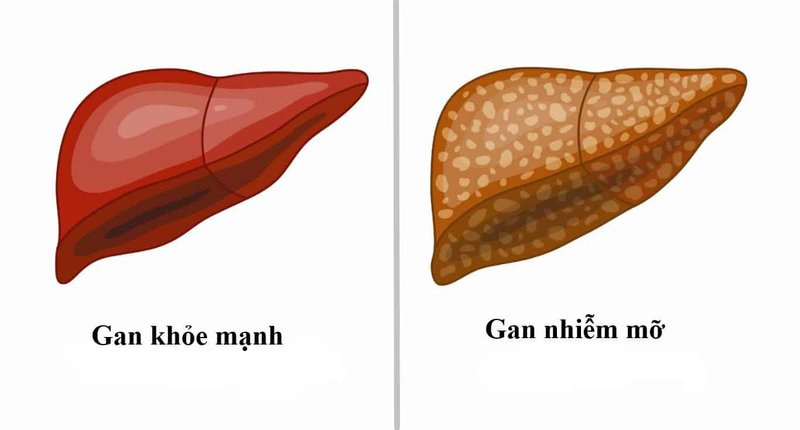
Bệnh nhân bệnh gan nhiễm mỡ không do rượu giảm cân sẽ cải thiện kết quả thận
Glucagon-like peptide 1 receptor agonist: Among its many mechanisms of action, glucagon-like peptide 1 (GLP-1) supports increased insulin secretion, delayed gastric emptying, and decreased appetite , all of which can lead to improved glycemic control and weight loss. In addition, an anti-inflammatory mechanism may make GLP-1 an attractive agent in nonalcoholic fatty liver disease and nonalcoholic steatohepatitis.
For example, GLP-1 Liraglutide, when compared with placebo, resulted in histological resolution of nonalcoholic steatohepatitis; however, larger studies are still needed. In chronic kidney disease, GLP-1 was shown to be nephroprotective, possibly due to GLP-1's ability to lower blood pressure in addition to the aforementioned mechanisms. GLP-1 inhibitors and SG2 liver transplantation have cardioprotective effects, and as discussed previously, patients with NAFLD and chronic kidney disease are at increased risk for adverse events. CV. Therefore, the use of these agents is recommended in patients with nonalcoholic fatty liver disease and chronic kidney disease. However, while there are landmark data to support the use of GLP-1 and SG inhibitors for liver transplantation to prevent CV events in CVD patients, data on the Primary prevention in patients with nonalcoholic fatty liver disease and chronic kidney disease is still lacking [ 103, 104] . Nevertheless, in patients with type 2 diabetes, chronic kidney disease, and nonalcoholic fatty liver disease, a liver transplant SG-2 inhibitor or GLP-1 is recommended not only for glycemic control but also for cardioprotective effects, liver and kidney.
Coenzyme Q10: Endogenously produced Coenzyme Q10 (CoQ10) has antioxidant and anti-inflammatory effects. CoQ10 also serves as an electron carrier in cellular respiration and as a cofactor in pyrimidine synthesis for DNA repair and replication, among other important roles. Patients with nonalcoholic fatty liver disease, chronic kidney disease and/or CVD have been reported to have CoQ10 deficiency [106]. The majority of endogenous CoQ10 is produced in the liver, and patients with nonalcoholic fatty liver disease have reduced CoQ10 production. CoQ10 deficiency will lead to oxidative stress, which serves as a major pathogenic factor in non-alcoholic fatty liver disease. Results from separate trials evaluating oral CoQ10 supplementation in patients with nonalcoholic fatty liver disease and chronic kidney disease.
In summary, CoQ10 has been shown to improve nonalcoholic fatty liver disease parameters and chronic kidney disease parameters in separate trials. CoQ10 also has a positive effect on the progression of cardiovascular disease, which is notable because patients with chronic kidney disease and non-alcoholic fatty liver disease are at increased risk for cardiovascular events. Supplementation may be beneficial in nonalcoholic fatty liver disease patients with chronic kidney disease, but clinical data on this population are lacking. Experimental Interventions Thiazolidinediones: Thiazolidinediones are agonists of the proliferating peroxisome-activating receptor (PPAR), and they play a physiological role in cell metabolism and differentiation. PPARs have been shown to be clinically useful in diseases such as hyperlipidemia (PPARα) and T2DM (PPARγ). Because chronic kidney disease is a manifestation of a metabolic and/or inflammatory process, the use of PPAR agonists has been studied in patients with chronic kidney disease. Specifically, pioglitazone, a PPARγ agonist, has been shown to improve cardiovascular outcomes in patients with chronic kidney disease and diabetes. Several RCTs have shown beneficial effects of pioglitazone on histopathology and metabolic function in patients with nonalcoholic steatohepatitis. Pioglitazone has been approved as a pharmacological agent in biopsy-proven nonalcoholic steatohepatitis by the American Association for the Research of Liver Diseases. Rosiglitazone was shown to improve the histological components of nonalcoholic steatohepatitis through an increase in insulin sensitivity while also improving liver function in a separate study, although neither study showed improvement in liver fibrosis. Interestingly, an extensive trial found that rosiglitazone was beneficial only during the first year of treatment, with no significant benefit observed with longer use.
However, Rosiglitazone is not available in most countries and its use is limited in the United States due to data regarding increased coronary events. The most widely studied PPAR agonist, Pioglitazone has shown favorable outcomes in patients with chronic kidney disease and in patients with nonalcoholic fatty liver disease, but there is a lack of data evaluating efficacy in patients with renal disease. chronic and non-alcoholic fatty liver disease.

Thiếu vitamin D gẩy ảnh hưởng đến bệnh gan nhiễm mỡ không do rượu và cũng liên quan đến bệnh thận mãn tính
Vitamin D: Vitamin D deficiency is associated with increased severity of nonalcoholic fatty liver disease and is also associated with chronic kidney disease. These findings could be explained by the physiology of vitamin D activation, which requires both renal and hepatic hydroxylation, and thus the presence of chronic kidney disease and non-fatal fatty liver disease. Alcohol certainly leads to vitamin D resistance. Furthermore, experimental models have demonstrated a role for hypovitaminosis D in the pathogenesis of both chronic kidney disease and nonalcoholic fatty liver disease.
In patients with chronic kidney disease, the therapeutic significance of vitamin D supplementation was higher indicating its ability to correct vitamin D deficiency, but a meta-analysis showed a higher prevalence of hypercalcaemia. In patients with nonalcoholic fatty liver disease, vitamin D supplementation does not correct vitamin D deficiency, however, trials are underway to evaluate the use of vitamin D supplementation in chronic kidney disease and nonalcoholic fatty liver disease/nonalcoholic steatohepatitis (NCT00893451, NCT01623024 and NCT02098317, www.clinicaltrials.gov ).
Probiotics: In rodent models, fecal microbiota transplantation, antibiotics in a fructose fed model reduced the severity of NAFLD, in when specific probiotics (Lactobacillaceae or Bifidobacteria) reduced proteinuria and decreased systemic inflammation in rodents with chronic kidney disease. While much of this data is based on studies from animal models, human trials are needed to further evaluate the therapeutic effects of the gut-liver-kidney axis.
2. Liver transplantation for patients with nonalcoholic fatty liver disease/nonalcoholic steatohepatitis and chronic kidney disease
In recent decades, nonalcoholic steatohepatitis has become more common and will become the most common indication for liver transplantation. Patients with nonalcoholic steatohepatitis have a higher incidence of chronic kidney disease than with other causes, and therefore, nonalcoholic steatohepatitis is rapidly growing as a cause for not only liver transplantation but also concomitant liver-kidney transplantation (SLKT) in the United States for serum creatinine. and dialysis status are important components of the end-stage liver disease (MELD) scoring model. Considering the increased prevalence of renal dysfunction in liver transplants due to preference based on the MELD allocation system in the United States, the prevalence of SLKT increased from 2.7% of all liver transplants in 2000 to 9.3% in the year 2000. 2016. Non-alcoholic steatohepatitis is currently the leading and fastest-growing indicator for SLKT in the United States with a 200% increase in SLKT from 2002 to 2010.
Để đặt lịch khám tại viện, Quý khách vui lòng bấm số HOTLINE hoặc đặt lịch trực tiếp TẠI ĐÂY. Tải và đặt lịch khám tự động trên ứng dụng MyVinmec để quản lý, theo dõi lịch và đặt hẹn mọi lúc mọi nơi ngay trên ứng dụng.