This is an automatically translated article.
The article is professionally consulted by Master, Doctor Nguyen Thi Thanh Thuy - Endocrinologist - Dialysis - Kidney Transplant - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital. The doctor has more than 15 years of experience in the diagnosis and treatment of medical kidney disease, hemodialysis, peritoneal dialysis, pre-transplant screening and post-transplant follow-up.Chronic glomerulonephritis is a disease that damages the glomeruli and progresses slowly over many years. The final stage of the disease leads to chronic kidney failure that gets worse and worse, seriously affecting the patient's health.
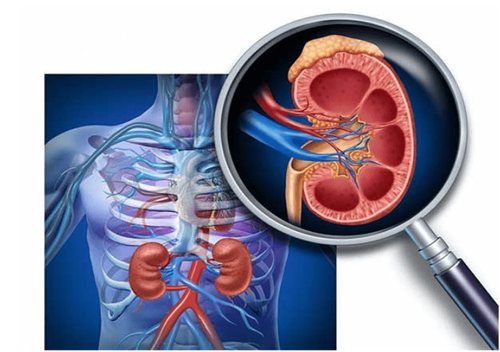
Chronic glomerulonephritis is a disease that causes damage to the glomeruli, which progresses slowly over many years.
1. What is the definition of chronic glomerulonephritis?
Chronic glomerulonephritis is a process of physical damage that occurs in all glomeruli on both sides of the kidney, including proliferation, edema, exudation and necrosis of hyaline, partial or total fibrosis. glomerulus set. The disease progresses slowly over many months and years, leading to atrophy of both kidneys.Clinical manifestations of chronic glomerulonephritis are diverse, there may be no prominent symptoms. Common symptoms are: edema, proteinuria, erythrocytosis, increased blood pressure. The disease progresses in stages, after 10-15 years, irreversible chronic kidney failure will appear.
Today, chronic glomerulonephritis is considered as a syndrome - that is, chronic glomerulonephritis syndrome. Chronic glomerulonephritis syndrome can be seen in many different histopathological lesions.
Histopathological lesions such as mesangial proliferative glomerulonephritis, membranous glomerulonephritis, membranous proliferative glomerulonephritis, focal glomerulosclerosis, extracapillary proliferative glomerulonephritis can all develop in general alike. But the rates of clinical syndromes vary. There are histopathological lesions that manifest clinically mainly as nephrotic syndrome, but others present with proteinuria and erythrocytosis without clinical symptoms.
Chronic glomerulonephritis includes 4 clinical forms:
Acute glomerulonephritis syndrome. Chronic glomerulonephritis syndrome. Nephrotic syndrome. Abnormal changes in urine (proteinuria, erythrocytosis without clinical symptoms). The above four clinical forms change alternately during the progression of the disease, lasting for months and years, and the final outcome is chronic kidney failure.
2. How does chronic glomerulonephritis form?
Có nhiều trường hợp viêm cầu thận mạn không rõ nguyên nhân khởi đầu
Focal, segmental proliferative glomerulonephritis: This inflammation occurs in part of the glomerulus or the whole glomerulus, with damaged glomeruli interspersed with intact glomeruli. Most focal proliferative glomerulonephritis is an IgA-induced glomerulonephritis. Clinical manifestations are cyclic hematuria, occurring after an upper respiratory tract infection and proteinuria ≈ 1g/24 h, usually without edema, without hypertension.
Focal, segmental glomerular fibrosis: Histopathological features are fibrosis, partial or total glomerular hyalinization without cell proliferation. Lesions first appear in the glomeruli in the paramedullary region and gradually spread to the entire cortex. Injured glomeruli are interspersed with normal glomeruli. In the renal interstitium, there is tubular atrophy, local inflammatory cell infiltration, immunofluorescence (+) with IgM and C3 in the damaged area. Approximately 90% of cases of focal glomerulosclerosis present with nephrotic syndrome.
Membranous glomerulonephritis: The histopathological feature of the disease is thickening of the glomerular basement membrane due to immune complexes deposited on the outside of the glomerular basement membrane under the epithelial surface, simple thickening of the basement membrane, no hyperemesis gravidarum. glomerular cell production. About 80% of cases of membranous glomerulonephritis have clinical manifestations with nephrotic syndrome, the rest are manifested by chronic glomerulonephritis syndrome or proteinuria, erythrocytosis without clinical symptoms.
Proliferative membranous glomerulonephritis: Histopathological features are proliferation of mesangial cells, mesangial organization combined with immune complex deposits in and out of the subepithelial membrane, in the intercellular space. circuit and also on the basement membrane. About 60% of cases of proliferative membranous glomerulonephritis have nephrotic syndrome, the rest are clinically manifested as chronic glomerulonephritis syndrome, acute glomerulonephritis syndrome or proteinuria, no red blood cells in the urine. clinical symptoms.
Extracapillary proliferative glomerulonephritis: The clinical manifestation of the disease is mainly acute glomerulonephritis, the most prominent sign is oliguria, acute renal failure progressive in episodes. The disease progresses to irreversible chronic kidney failure, and the patient usually dies within 6 months to 2 years. Extracapillary proliferative glomerulonephritis is also known as rapidly progressive glomerulonephritis, also known as malignant glomerulonephritis.
2.2. Secondary chronic glomerulonephritis Secondary chronic glomerulonephritis occurs after a variety of medical conditions. The causes of chronic glomerulonephritis are diverse. The main causes are:
Collagenose-induced glomerulopathy:
Systemic lupus erythematosus: is an autoimmune disease, common in women, very rare in men. About 80-100% have chronic glomerulonephritis and nephrotic syndrome. The majority of patients with systemic lupus erythematosus die from end-stage renal failure.

Bệnh nhân lupus ban đỏ hệ thống thường bị tử vong do suy thận giai đoạn cuối
Inflammation of small nodular microvasculature. Wegener's Granulomatosis Rheumatoid Hemorrhage Goodpasture's syndrome:
Clinical presentation is hemoptysis, possibly massive hemolysis leading to death, associated with chronic glomerulonephritis and often extracapillary proliferative glomerulonephritis. .
Diabetes mellitus: Clinical manifestations are chronic glomerulonephritis syndrome, nephrotic syndrome, benign renal arteriosclerosis or malignant renal artery fibrosis. End-stage renal failure is one of the leading causes of death in diabetes.
Infectious glomerulonephritis:
Glomerulonephritis caused by hepatitis viruses Subacute endocarditis (osler disease) Chronic glomerulonephritis caused by malaria, leprosy, syphilis. Toxic glomerulonephritis:
Gold salt toxicity Penicillamine toxicity Chronic glomerulonephritis due to abnormal protein deposition:
Light chain nephropathy Heavy chain nephropathy. Waldenstrom's disease primary globulin amyloidosis and secondary amyloidosis. Glomerulonephritis due to malignancies:
Acute leukemia, chronic leukemia, ganglion sarcoma, Kahler's disease.
3. Prevention of glomerulonephritis

Vệ sinh miệng họng sạch sẽ cũng là một cách phòng bệnh
When you suspect you have the disease, you need to go to a reputable medical facility immediately. Limiting to diseases of pharyngitis, boils, impetigo (these are the causes of acute glomerulonephritis). Need to clean personal hygiene to avoid skin diseases (acne, boils...) Vaccinate against hepatitis B, do not share needles. Periodic medical examination every 6 months (including blood tests to evaluate kidney function and total urinalysis). We hope that the above information helps you better understand chronic glomerulonephritis as well as its causes. You should also have regular health check-ups so that you can detect the disease at the earliest and treat it early if there is a disease.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.













