This is an automatically translated article.
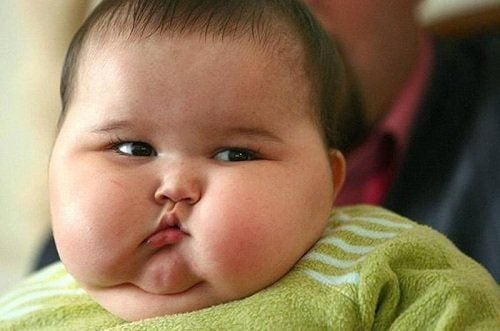
Post by Master, Doctor Ma Van Tham - Pediatrician - Department of Pediatrics - Neonatology - Vinmec Phu Quoc International General Hospital.Obesity is a very important problem not only in developed countries but also in developing countries like Vietnam. According to the Ministry of Health, the obesity rate among children 6-11 years old in the inner city of Ho Chi Minh City is now 12%, Hanoi is 8-9%. Obesity and its consequences are increasingly a risk factor for public health.
1. Definition
According to the World Health Organization WHO
- Overweight is a condition in which the body's energy exceeds the energy it should have compared to height.
- Obesity is a condition in which the body accumulates excessive fat, locally or globally, to the extent that it adversely affects the health of the body.
2. Obesity classification
2.1. Classification by etiology Simple obesity: The type of obesity without a clear pathogenesis accounts for more than 90%.
Pathological obesity: Due to endocrine diseases or genetic defects 10%
2.2. Classification according to adipose tissue morphology and age of onset of obesity Early onset obesity: Present before the child is 5 years old.
Late onset obesity: Late onset obesity after 5 years of age.
The most likely stages of obesity are infancy, 5-7 years old, and adolescence. Obesity that occurs during this stage increases the risk of chronic obesity and complications such as cardiovascular disease risk and psychiatric disorders than late-onset obesity.
2.3. Classification by segmentation of adipose tissue and anatomical location Abdominal obesity (central fat, upper body fat, apple fat, male fat): Fat is concentrated in the abdomen.
Thigh fat (peripheral fat, low fat, pear-shaped fat, female fat): Fat is concentrated mainly in the buttocks and thighs.
Belly fat has a higher risk of cardiovascular disease, diabetes, hyperinsulinemia, dyslipidemia, glucose intolerance than thigh fat.

3. Causes of pathological obesity
3.1. Endocrine obesity Obesity due to hypothyroidism: Uncommon causes (1/350). Late onset obesity, moderate obesity, slow growth, dry skin, constipation, mental retardation.
Obesity due to hyperadrenocorticism (HC Cushing): Caused by pituitary or adrenal cortex, the most common is drug-induced Cushing's syndrome. Fat in face and body, red face, burgundy stretch marks, early genital hair growth, slow growth.
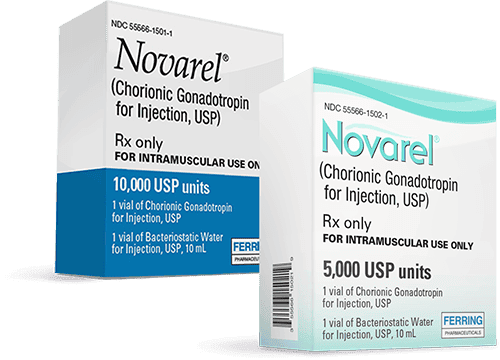
Obesity due to lack of growth hormone GH: Obesity is localized in the chest area, in the trunk, height is clearly reduced. May be associated with deficiency of anterior pituitary hormones such as ACTH, TSH, FSH, LH.
Obesity due to lesions of the hypothalamus - pituitary gland: These lesions cause appetite, common in boys.
3.2. Obesity due to multiple malformation syndrome Willi - Prader - Labhart syndrome: A common cause. Generalized obesity due to overeating appears early from 3 to 4 years old, facial deformities (narrow forehead, hooked nose), small head and limbs, decreased muscle tone, dwarfism, mental retardation, possibly diabetes , hypogonadism. Usually due to a deletion on chromosome 15 (50%).
Laurence - Moon - Biedi syndrome: Early obesity is often associated with mental retardation, polydactyly, retinitis pigmentosa appearing later than 10-12 years of age. Hypogonadism due to decreased gonadal hormones. Inherited recessive, autosomal recessive.
Astrom syndrome : Obesity with diabetes, deafness, retinitis, hypogonadism. Inherited autosomal recessive disease.
Biemon syndrome: Obesity with nail defects, polydactyly, hypogonadism. Autosomal recessive inheritance.
Borjson syndrome: Obesity, short stature, rough face, hypogonadism.
3.3. Risk factors for exogenous obesity Family and genetic factors: Many cases of obesity have a family history. Children with obese parents can become obese at any age: By age 17, the rate is three times higher than in families with non-fat parents. Among obese children, about 80% of children have one parent. obese, 30% have both parents obese. Reduced physical activity: Lack of physical activity is the main source of obesity because obesity leads children to lead a sedentary lifestyle. Sleep less: Studies show that children who sleep less than 8 hours / day and night have an increased risk of obesity when they are over 15 years old. Sleep less but go to bed early, watch TV for many hours, reduce physical activity... The sleep of obese children can be disturbed due to fluctuations in hormonal factors such as serotonine. Breast milk is a protective factor in preventing obesity: Studies have shown that breast milk also has a preventive effect on obesity in children: The less time breastfed, the higher the risk of childhood obesity. Premature fat accumulation is a risk factor for childhood obesity. BMI increases rapidly during the first year, then gradually declines to a lowest level between 4 and 8 years of age (average age 6 years) and then gradually increases until adulthood. The return of BMI during infancy is termed early fat storage. Premature fat accumulation before age 5.5 is a risk factor for childhood obesity. Therefore, values of BMI before and during the fat storage phase must be determined to accurately assess risk progression. Psychological and emotional factors: Psychological and emotional factors are risk factors for childhood obesity. The lack of parental care and education during childhood is a risk factor for obesity. Precocious puberty and obesity: Research shows that 30% of overweight girls and 15% of obese girls get their period before age 11
4. Dangerous consequences of obesity
Psychophysiological disorders and social inclusion : There is a correlation between the degree of obesity and signs of anxiety, depression, attitude and behavior disorders, self-satisfaction, and academic scores as well. decline, there is a link between fear of being overweight and depression, especially in girls.
Precocious puberty: There is a link between obesity and early puberty.
Consequences of physical beauty disorders: In boys, there is a condition of large breasts. In girls, early menstruation, hirsutism, acne. Both sexes: Body deformity, big belly, white or purple stretch marks.
Metabolic disorders
Blood sugar disorders: There is a close correlation between the level of increased insulin, increased proinsuline and % of fat mass in prepubertal and pubertal obese children. This can cause hirsutism in girls. Type 2 diabetes: Increased prevalence of type 2 diabetes in overweight (BMI > 85er percentil) adolescents with obesity and reduced physical activity. Dyslipidemia: There is a correlation between obesity and hypercholesterolemia. Cardiovascular complications, hypertension: All studies have concluded: In obese children with high arterial blood pressure, the mean blood pressure is significantly higher than in non-obese children.
Respiratory complications: The prevalence of obesity is high in children with asthma.
Sleep apnea and nocturnal respiratory disorders: Research in the US shows that 27% of obese children have severe and moderate sleep apnea.
There are also gastrointestinal complications (fatty liver), neurological complications (benign cranial hypertension syndrome), orthopedic complications (curvature of the spine, bent legs) also increased in children. fat.
Long-term consequences
Obesity in adults: Childhood obesity can lead to long-term consequences of obesity in adults: 20-50% chance of prepubertal obesity by 50 - 75% obese after puberty. Risk of multiple cardiovascular diseases and metabolic syndrome in adulthood: Cardiovascular risks in obese children such as high blood pressure, dyslipidemia, metabolic syndrome persist into adulthood.

5. Studying the effectiveness of childhood obesity treatments
Studies conducted on treatment modalities include
Diet. Exercise physical activity Psychological treatment. Coordinate with other interventions. 5.1. Efficacy of diet and increased physical activity Diet to limit sugar, limit lipide, Encourage eating grains, vegetables, fruits. Limit the number of meals: 4 times/day including snacks. Physical activity 40-55 minutes / time for jogging or aerobic exercise 2 - 5 times / week for 4 - 8 months reduce % fat mass.
5.2. Psychotherapy and supportive treatments A combination of psychotherapy, diet and physical activity over a long period of 24 months results in significant weight loss in children <12 years of age.
In older children, psychological education and low-calorie diets and light exercise produce good results.
5.3. Use of drugs and surgical treatment There are some studies but not enough to conclude the effectiveness of drugs and surgical treatment (surgery) in the treatment of childhood obesity.
REFERENCES
ANAES( 2003), Prise en charge de l'obesite de l'enfant J.Ph. Girardet, P. Tounian.(1997), “L’examen de l’enfant obeseˮ, La enterprise en charge therpeutigueˮ, Dossier: L’obesiste de l’enfant. Realites Pediatrique, N 20. WHO(1997), “Obeseste: Preventing and managing the global epidemic”, Report of a WHO Consuntation on Obesity. WHO (2000) Technical Report Series 894, Obesity: Preventing and managing the global epidemic. WHO (2001), The world of WHO in the Western Pacific Region: Report of the Regional Director.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.