This is an automatically translated article.
Blood is a special probiotic. Blood is also considered a medicine, when it is necessary to use it according to the indications. Because blood transfusion also has potential risks of unforeseen complications. Therefore, some of the following principles when blood transfusion should be strictly followed to help ensure the safety and life of the patient.
1. Principles of blood supply
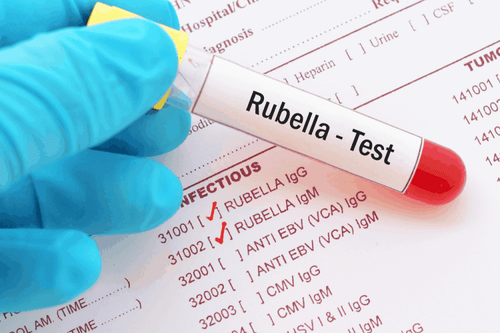
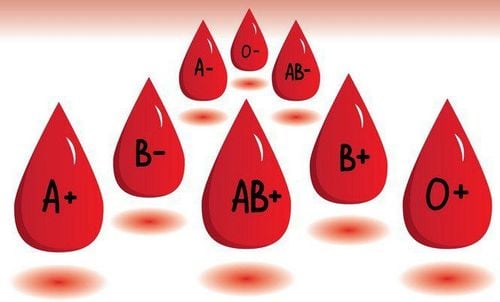
Blood units distributed at the blood storage room for medical staff of the clinical department to receive for transfusion must ensure that necessary basic tests have been performed such as ABO blood group determination, Rhesus and infectious diseases such as HIV, hepatitis B, C, malaria, syphilis and CMV.
Medical staff will only receive blood when it has been done and the result is an immune concordance of blood group between the blood unit and the patient right at the blood reserve room.
Not dispensing, not receiving and using blood units with visible signs such as perforation, opening, or rupture on the blood bag or the insertion site of the transfusion set; there is layering or clumping, precipitation, scum or change in color of blood...
2. Principles of blood transfusion

Bác sĩ điều trị cần thăm khám và đánh giá tình trạng bệnh lý, phát hiện sớm nhu cầu cần truyền máu ở người bệnh
The treating doctor needs to examine and evaluate the patient's medical condition, early detect the need for blood transfusion in the patient.
The treating doctor must order the ABO, Rhesus blood group test for the patient who is expected to need a blood transfusion and make a blood plan.
Indications for blood transfusion are made after weighing the potential benefits of blood transfusions to outweigh the possible risks from blood transfusions.
Patients or family members need to be consulted by a doctor about the benefits and possible risks of blood transfusion. Blood transfusions can only be done with the written consent of the patient or family member. However, in cases of urgent need for blood transfusion without the patient's consent, the doctor must prescribe it and specify it with the confirmation of another medical staff in the medical record.
3. Principles of preparation before blood transfusion
Check and compare the received blood sample information with the estimate sheet. Always test to ensure transfusion immunocompatibility between the patient's blood sample and the blood bag at the patient's bed. The clinician is responsible for reading blood group matching results and for making transfusion decisions. Transfuse blood immediately after thawing, avoid leaving the blood bag in the normal environment for too long.
4. Principles of performing and monitoring blood transfusion
Check and compare necessary contents such as patient information and blood unit information such as blood product type, blood type, code number and expiry date.
When performing blood transfusion, patients need to be closely monitored for developments in order to alert nurses and doctors to early detection and timely treatment of complications related to blood transfusion.
The patient's pulse, temperature, blood pressure, and mental status are recorded at the time before and during the blood transfusion, clearly recorded in the blood transfusion record or monitoring sheet. In particular, during the first 15 minutes, special attention should be paid to monitoring because blood transfusion complications are very common during this period.
Must use a dedicated line for blood transfusion.
Blood transfusion line is an independent line, absolutely do not share the same line with other drugs. In addition, the blood bag contains only the transfused blood, and nothing should be added to the blood bag, except when isotonic saline solution is indicated to dilute the erythrocyte sedimentation during transfusion.

Phải sử dụng bộ dây truyền chuyên dụng để truyền máu
5. Principles of handling when complications related to blood transfusion occur
Any abnormality occurs during blood transfusion, the transfusion should be postponed immediately. The nurse checks the patient's condition, including vital signs, and immediately reports it to the attending physician.
The doctor needs to identify each case with the level and cause of the abnormalities to decide whether to stop the blood transfusion or reduce the rate.
If there is an indication to completely stop the blood transfusion, this intravenous line should continue to be maintained with isotonic saline, ready access when there is a problem.
If the patient has an emergency situation, it is necessary to treat the patient according to the issued protocol. Then, the doctor needs to report the incident to the management.
If delaying blood transfusion for more than 4 hours or not eliminating the possibility of a transfusion-related accident, this blood unit needs to be destroyed according to the patient regulations, not allowed to continue to be transfused to another person. sick.
6. Principles of monitoring after blood transfusion
Based on the patient's condition and the progress in the blood transfusion process, the treating doctor appoints monitoring after the end of the blood transfusion. If the blood transfusion is favorable, the patient should monitor vital signs after the first hour of transfusion. After that, return to the same care regimen as before blood transfusion. Recheck indications for blood transfusion and perform blood planning if indicated. If an accident occurs during a blood transfusion, the monitoring regimen depends on the patient's condition. The number of transfused blood transfusion units and the type of preparations used should be clearly stated in the hospital discharge papers for convenience in tracking and tracing later. In short, blood is a very special "medicine", which cannot be produced but is obtained thanks to the donor. Therefore, the blood source is extremely precious and blood transfusion must always be strictly indicated and adhered to a number of principles, both to ensure the safety of the patient, and to prevent serious related complications.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.