This is an automatically translated article.
The article was written by MSc Vu Duy Dung - Doctor of Neurology, Department of General Internal Medicine - Vinmec Times City International General Hospital.Metastatic tumors are the most common tumors of the spinal cord and can be epidural, pleural, or, rarely, intramedullary. Spinal cord compression due to epidural metastases is a neurological emergency and should be diagnosed quickly because the pre-treatment neurological status has a great influence on the post-treatment outcome.
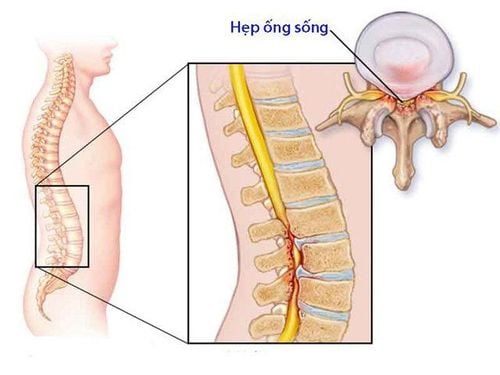
1.Spine metastatic tumors Metastatic tumors of the spine are tumors that originate outside the central nervous system and spread hematogenously or invade directly from surrounding adjacent structures. Spine. They are the most common tumors in the spine. These tumors can be classified as epidural, medullary medullary or intramedullary metastasis:
Epidural metastasis
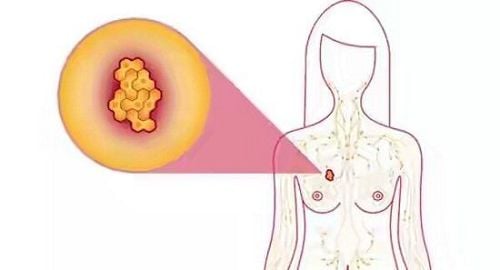
Lung Breast Prostate Thyroid Kidney Pleural Metastasis
Breast Lung Gastric melanoma – bowel Intramedullary metastasis
Lung Breast Melanoma In addition, we will also cover primary brain tumors that often spread to the spinal canal, including:
Myeloblastoma Embryonic tumors with multilayered rosettes Neuroblastoma of the central nervous system Meningiomas Ventricular tumors High-grade glioma Primary lymphoma of the central nervous system
2. Tumors that have metastasized from outside the central nervous system With the improvement in cancer treatment around the world, patients with advanced cancer will live longer; Consequently, there will be an increase in the number of spinal metastases. After the lungs and liver, bone is the third most common site of metastasis. The spine is the most common site of bone metastases.
Trắc nghiệm: Thử hiểu biết của bạn về bệnh ung thư
Ung thư là nguyên nhân gây tử vong hàng thứ 2 trên thế giới. Thử sức cùng bài trắc nghiệm sau đây sẽ giúp bạn có thêm kiến thức về yếu tố nguy cơ cũng như cách phòng ngừa bệnh ung thư.
Bài dịch từ: webmd.com
2.1 Epidural Spinal Metastases Lung, breast, prostate, thyroid, and kidney cancers account for the majority of spinal metastases. Epidural metastases are the most common form of spinal metastasis and usually involve the vertebrae (85%), followed by perivertebral tissue (10% to 15%), and, rarely, the epidural body. Epidural metastases are common in the thoracic spine (60%), the sacral and cervical spine (10%), and multiple spinal segments (30%). Because the bone marrow is rich in blood vessels, most vertebral metastases occur in the vertebral body. Such metastatic masses develop posteriorly in the epidural space and can lead to spinal cord compression from the epidural. The most common presentation is periaxial pain and progresses because of direct invasion of the tumor into the membrane. vertebral body and surrounding soft tissue, resulting in mechanical compression of the spinal cord. The dura mater is a strong anatomical barrier and is rarely penetrated. Periaxial pain may differ from normal back pain because it is unrelated to movement and posture, does not abate with rest, does not respond to conservative treatment, and is progressive. Nocturnal pain and soft percussion are poor prognostic signs. Nocturnal pain due to epidural venous plexus congestion. Bone invasion can cause pathological fractures, spinal instability, and scoliosis. If the spine is unstable, pain may worsen with strenuous movement. Acute pain usually indicates a pathological fracture. Most patients will have spinal and radiculopathy. Circular muscle dysfunction on admission is less common and occurs in about 3% of patients. The most feared complication of spinal metastasis is epidural compression, which occurs in 5% to 10% of patients during the course of the procedure. pathology and is a neurological emergency where delay in treatment leads to severe and irreversible neurological complications. In addition, pretreatment neurological status predicts post-treatment outcome, making early diagnosis even more important. Spinal cord compression above the spinal cone causes symptoms of upper motor neuron weakness, although in the episode of spinal shock there may be flaccid paralysis resembling lower motor neuron damage. Loss of sensation begins in the toes and usually spreads upward, eventually reaching one to five segments of the pulp below the level of pulp compression. Therefore, sensory levels cannot be used to precisely localize the lesion. Vibration and postural sensations are soon lost, followed by pain and heat sensations. Patients may present with medullary cone syndrome, with acute symptoms of saddle sensory loss, marked and early circular muscle dysfunction, and a combination of superior and inferior motor neuron weakness. If there is compression of the caudal nerve roots, lower motor neuron weakness in the legs will appear, along with a segmental sensory deficit, sciatica, and bladder dysfunction and intestine in late stage. If an epidural spinal metastasis is suspected, an MRI of the entire spine should be performed, as one-third of patients will have multiple foci of which clinical examination is not reliable enough for adequate localization. CT of the spine may also be useful to examine the bones of the spine, especially if there are signs of axial instability.
Treatment is aimed at minimizing or reversing neurological symptoms. Corticosteroids are used to reduce spinal edema. A loading dose of dexamethasone of 10 mg to 100 mg is usually used, followed by gradual dose reduction. In a randomized study of 37 patients and in another non-controlled case series of 28 patients treated with high-dose dexamethasone (96 mg to 100 mg IV) as a loading dose, there was no apparent benefit. of high-dose dexamethasone compared with low-dose dexamethasone (10 mg to 16 mg). If neurological signs and symptoms are minimal, a loading dose of 10 mg dexamethasone followed by 16 mg/day in 4 divided doses may be used. Patients with spinal instability, localized lesions, and favorable prognosis are treated with a combination of surgery and then radiotherapy. Anterior decompression and spinal reconstruction is a reasonable approach, rather than posterior archectomy. Posterior arcectomy has fallen out of favor as the majority of epidural tumors are located in the anterior vertebral bodies and cannot be accessed by posterior entry. Radiation therapy should be initiated quickly, especially when surgery is contraindicated. Radiation therapy can be given as short-term radiotherapy, long-term radiotherapy, or localized body radiotherapy. Localized radiotherapy allows for higher doses of radiation to be delivered to the target while minimizing radiation exposure to adjacent tissues and is now commonly used to treat metastatic spinal tumors. Proton therapy has a similar advantage in terms of its ability to protect nearby organs; however, proton therapy is not available everywhere, and there is no group I evidence to support its use.
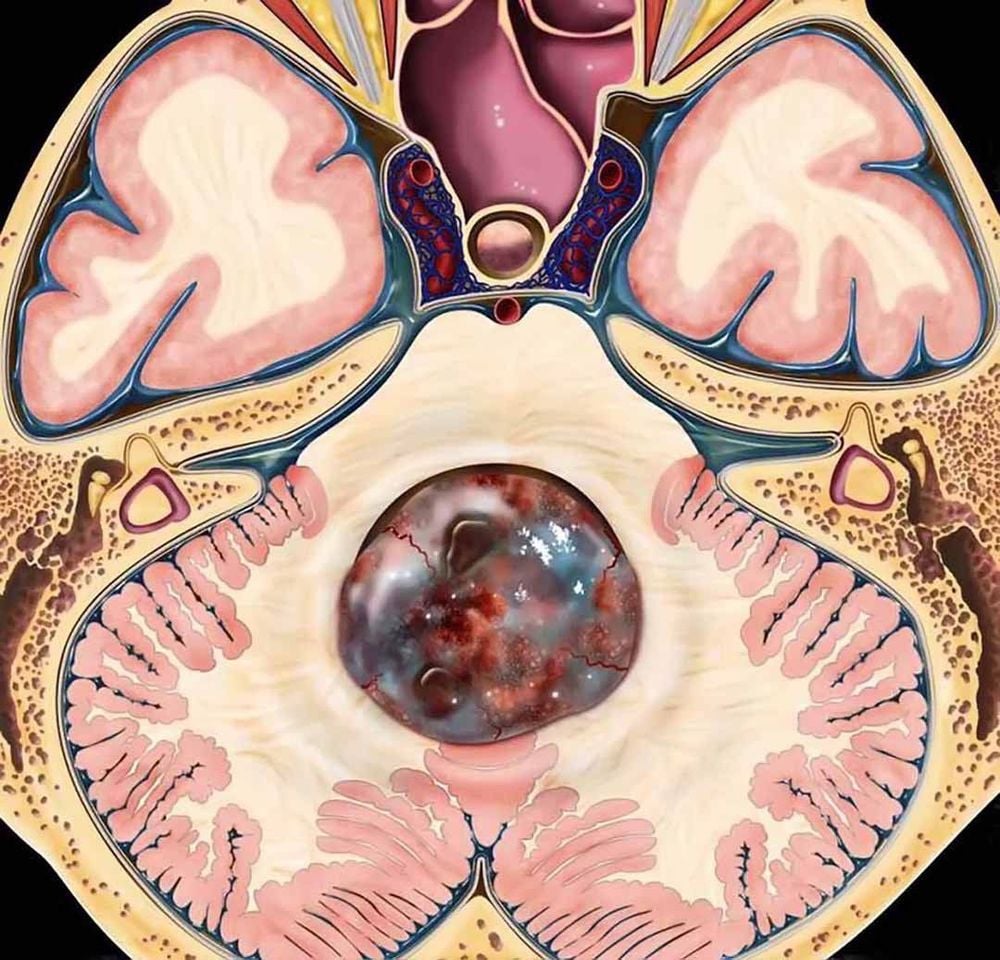
2.2 Muscular metastases Soft membrane metastases, also known as neoplastic myelitis, are caused by cancer cells metastasizing to any part of the central nervous system that comes into contact with fluid. cerebrospinal fluid and seed and grow along the medulla oblongata. Tumor cells can spread to the soft pulp membrane single-focal, multifocal and diffuse. Pleural myelopathy is often associated with advanced cancer, and most patients have a large systemic burden of cancer. Breast cancer, lung cancer, melanoma, and gastrointestinal cancers account for the majority of medulloblastoma cases. When medullary membranous metastasis occurs in the spine, tumor cells tend to be deposited in the ponytail due to gravity and decreased CSF circulation.
Symptoms are often multifocal and may be attributed to one or more of the following areas: cerebral hemispheres, cranial and brain stem nerves, or spinal cord. Patients may have headache, meningeal irritation, nausea, vomiting, diplopia, cerebellar dysfunction, back pain, and radiculopathy. When spinal cord involvement is predominant, patients will have lower motor neuron-type bipedal weakness, paresthesias, back pain, radicular pain, and bladder and bowel dysfunction. Weakness or paralysis of the extremities is a common first sign in patients with spinal cord injury. The combination of cytology and abnormal whole-axis MRI will confirm the diagnosis in most cases. In a clinical study of 48 patients with both cytology and whole-axis MRI, 54% had a confirmed diagnosis of myelopathy on both cytology and MRI, and 21% had positive MRI only. while 25% had only positive cytology with no abnormalities on MRI. In a similar study, imaging was higher in the diagnosis of pleural medullary metastases with solid tumors (88%) than with hemangiomas (48%). Cytological examination is equally valid for the diagnosis of membranous membranous metastases between solid tumors (85%) and hemangiomas (89%). MRI should be performed prior to lumbar puncture because lumbar puncture can cause a decrease in CSF pressure leading to increased meningeal and meningeal enhancement.
MRI of the spine may show increased parenchymal and subarachnoid enhancement nodules, diffuse or localized enhancement, and increased nerve root enhancement. If MRI is typical in a patient with a known metastatic disease, CSF cytology may not be necessary to confirm the diagnosis. Cerebrospinal fluid testing often has nonspecific findings such as increased open pressure (>20 cmH2O), leukocytosis (>5/mm3), increased protein (>50 mg/dL), and decreased glucose (<40 mg/dL). However, a definitive diagnosis cannot be made unless malignant cells are seen on cytology of the cerebrospinal fluid. A minimum of 4 mL and preferably 10 mL of CSF should be obtained and processed immediately to avoid false negatives. Malignant cells are only seen in the CSF in about 50% of cases on initial testing, and repeat lumbar puncture may be helpful. Treatment is usually intramedullary or intraventricular injection of methotrexate, liposomal Ara-C, topotecan, or thiotepa. Nodular metastases in the soft pulp membrane can be palliatively treated with radiotherapy. Pulmonary myelopathy portends a poor prognosis in cancer patients, and most patients have overall survival less than 6 months.
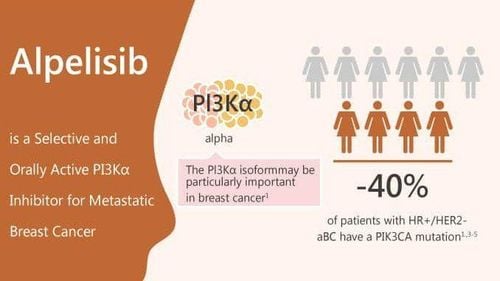
2.3 Intramedullary metastases Intramedullary cancer metastases are rare and account for only 0.5% of spinal metastases. The most common non-CNS cancers with intramedullary metastasis are lung cancer (48% to 54% of all intramedullary metastases), breast cancer (11% to 16%), and melanoma factor (6% to 8%). The cervical marrow is the most common site of metastasis (41% to 42%), followed by the lumbar spinal cord (32% to 38%) and the thoracic cord (26% to 34%).
3. Metastatic lesions from central nervous system tumours Metastatic lesions from primary brain tumors present as pleural medullary or trickling metastases. Drip metastases are nodular soft medullary metastases that extend downward through the CSF spaces from an intracranial tumor or spinal cord tumor. Drip metastases from intracranial tumors are usually extramedullary in the dura and have a preference for the caudal nerve roots. Myeloblastomas, meningiomas, primary CNS lymphomas, and, rarely, high-grade gliomas present with spread to the medulla oblongata. Despite their rapid progression, glioblastomas rarely spread to the cerebrospinal fluid. The incidence of pleural effusion from malignant glioma is approximately 2%, although autopsies reveal medullary medullary metastases in up to 21% of patients. Soft membranous dissemination of malignant gliomas is more common in children and young adults. Meningiomas have a higher propensity to diffuse to the spine than other CNS gliomas, and approximately 11% to 15% of patients have tumor dissemination.
Embryonic tumors such as myeloma, embryonal tumors with multilayered rosettes, and CNS neuroblastoma have metastases in one third of cases. Spinal metastases are found in up to 40% of myeloma cases and are most common in the lumbar-sacral and thoracic spinal cord. Therefore, cerebrospinal fluid testing and whole-neuraxial studies should be performed as part of routine evaluation. Soft-membranous dissemination is seen in 16% of patients with primary CNS lymphoma, and only a few cases (4%) are detectable on MRI.
Early cancer screening is considered a perfect measure in the timely detection and treatment of all types of cancer. Vinmec International General Hospital currently has a high-tech cancer screening and examination package, including genetic testing, imaging, and biomarkers for early tumor detection. A single gene test can assess the risk of 16 common cancers in both men and women (lung cancer, colorectal cancer, breast cancer, pancreatic cancer, cervical cancer) Bowel cancer , stomach cancer , prostate cancer ,....)
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Wu J, Ranjan S. Neoplastic Myelopathies. Continuum (Minneap Minn) 2018;24(2, Spinal Cord Disorders):474-496.
MORE:
Vascular diseases of the spinal cord (Part 1) Vascular diseases of the spinal cord (Part 2) Vascular diseases of the spinal cord (Part 3)