This is an automatically translated article.
Article written by MSc Hoang Van Lan Duc - Doctor of Radiology - Department of Diagnostic Imaging and Nuclear Medicine - Vinmec Times City International Hospital
Intra-abdominal ectopic pregnancy is often difficult to diagnose. In this case, ultrasound will not show the pregnancy in the uterus, no ectopic pregnancy in the bilateral appendage, it may be necessary to use computed tomography to find the pregnancy mass.
1. Points to note about the location of the ectopic pregnancy
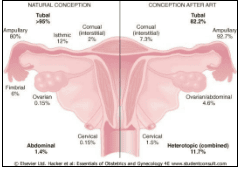
For natural pregnancy: the rate of ectopic pregnancy in the fallopian tube (fallopian tube) is the most common (> 95%), this is the location where the pregnancy mass causes the most typical symptoms, possibly rupture. cause intra-abdominal bleeding, if not diagnosed and treated promptly, can lead to death. Other sites are less common, such as in the abdomen about 1.4%, in the ovary about 0.15%. Mixed pregnancy has both ectopic pregnancy and intrauterine pregnancy with a very low rate, about 1/30000 cases. For cases with assisted reproduction (such as IVF): the rate of intra-abdominal and ovarian pregnancy is higher than that of natural pregnancy, with 4.6%. Mixed pregnancy occurs with the rate up to 11.7%.
2. Circumstances suggesting an ectopic pregnancy
In the case of a woman of childbearing age, there is sudden severe abdominal pain, possibly accompanied by abdominal fluid (if ultrasound is available), or a urine hCG test (+) A ruptured ectopic pregnancy should be considered immediately (until there is evidence that it is not an ectopic pregnancy), and requires emergency resuscitation, even immediate surgery. For the remaining cases, think of an ectopic pregnancy when there are the following signs: Clinical with the following 3 classic symptoms:
+ Abdominal and pelvic pain.
+ Menstrual disorders or amenorrhea.
+ Vaginal bleeding, there may be blood clots.
In addition, there may be other symptoms.
With natural pregnancy If the β-hCG test is available, with a level > 1500 mIu/ml and no intrauterine pregnancy, then an ectopic pregnancy should be considered. It is also important to note that the cut-off threshold for β-hCG varies from study to study, usually from 1000 to 2000 mIu/ml. If the cut-off is low, the risk of false positive (positive) ectopic pregnancy diagnosis is high. false negatives), if the threshold is high, it is easy to miss an ectopic pregnancy or make a delayed diagnosis (false negative).
With many studies showing that, with cases of suspected ectopic pregnancy, when monitoring, up to 90% will appear normal intrauterine pregnancy. With the rate of intrauterine pregnancy and ectopic pregnancy occurring in about 30000 pregnancies, so when ultrasound shows an intrauterine pregnancy, ectopic pregnancy can be ruled out to an acceptable level.
In the case of assisted reproductive technology (IVF) Counting the number of gestational sacs in the uterus is especially important. Because when doing IVF, usually at least 2 embryos are placed in the uterus. At that time, if the ultrasound shows not enough fetuses, the question to ask is, is it possible that the other embryo is saved, or can be pushed out of the uterus causing an ectopic pregnancy? Therefore, mixed pregnancy in the case of IVF is particularly high.
3. When does ultrasound diagnose an intrauterine pregnancy?
Because, in natural cases, if ultrasound shows a pregnancy in the uterus, it can rule out an ectopic pregnancy.
So when does the ultrasound conclude that the pregnancy is in the uterus?
Intrauterine pregnancy goes through the following stages:
The stage only shows the amniotic sac, the average diameter of the amniotic sac is about 5-7mm, the intrauterine sac sign (IDSS) can be seen. or double decidual sac sign (DDSS). This stage is about 4 to 4.5 weeks pregnant. Stage with yolk sac: the amniotic sac is about 10mm in size, with the same characteristics as above, but inside has a yolk sac shape. This stage of pregnancy is about 5-5.5 weeks. The stage of embryogenesis: the amniotic sac is the same as the one above, larger in size, in addition to the yolk sac, the embryo can be seen, and the fetal heart can be seen. This stage is at least 6-6.5 weeks pregnant.
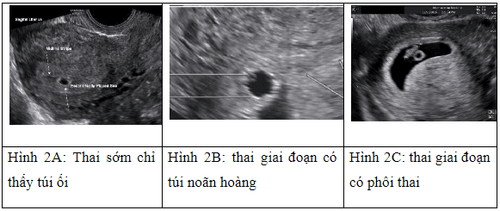
However, at the stage where only the amniotic sac is seen, with typical signs of hyperechoic border or double border sign, it also has low sensitivity and specificity (Sen 34 - 65%, spe 58 - 75%). , the value of negative diagnosis is low (12-18%).
That is, with an intrauterine outbreak with regular rounded margins (like pseudo-amniotic sac), but without signs of IDSS or DDSS, it is still possible that a gestational sac is present (needs to be associated with laboratory tests and follow-up ultrasound). As for the case of small amniotic sac, with IDSS/DDSS sign but no yolk sac or embryo, it is most likely a false amniotic sac encountered in ectopic pregnancy, and this case if subjectively not monitored, or if the patient conducts abortion, then it is very likely that the ectopic pregnancy will be missed, even thinking of complications of abortion without thinking about the symptoms of ectopic pregnancy.
Therefore, at this early stage should always be differential diagnosis with a pseudo-amniotic sac (can be seen in ectopic pregnancy - about 20%). And many authors advise, when ultrasound only concludes pregnancy when it shows the presence of a yolk sac or embryo, and in cases where only the amniotic sac-like shape is seen, with or without IDSS/DDSS signs, it is not. Therefore, it should be concluded that the pregnancy is early in the uterus, but it is necessary to rely on the β-hCG test and follow-up to make a diagnosis.
4. NICE Diagnostic Ultrasound Guide 2019
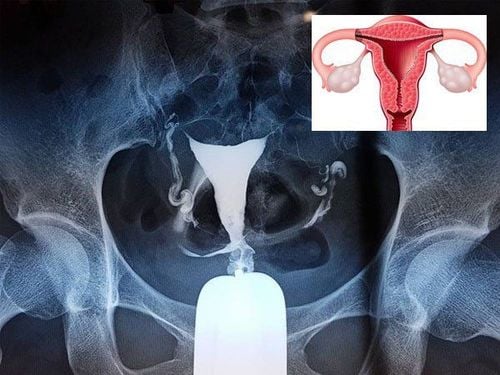
NICE 2019 guidelines for diagnostic ultrasound for ectopic pregnancy with tubal location (most common) as follows:
4.1 When the ultrasound shows the following images, it is concluded that the pregnancy is ectopic
See a mass in the adnexa, separate from the ovary (with transducer ultrasound, when the probe is pushed into the mass, it moves separate from the ovary), the presence of amniotic sac with the image of the ovarian sac is seen. Internal gynaecomastia (appears in about 8.3%), or
Sees the same mass as above but with more embryos, there may be fetal heart activity (occurs in about 7.4%).
When the above mass is seen, with the image of the fetus in the uterus, the diagnosis is mixed pregnancy (ectopic pregnancy with intrauterine pregnancy).
4.2. When seeing the following images, there may be a high rate of ectopic pregnancy, but it must be combined with clinical and β-hCG testing to diagnose.
An adnexal mass, separate from the ovary, internally shaped like an amniotic sac but without a yolk sac or embryo (empty amniotic sac), sometimes described as a ring with thick wall, on color Doppler seen angiogenesis “ring of fire” sign. (Seen in about 24.7%). Or
A mixed negative mass in the appendage, separate from the ovary. (Seen about 54%).
In this case, it is very important to differentiate an ectopic pregnancy from other lesions, such as ovarian tumor (usually seen before, no sign separate from the ovary, no sign of fire circle). ), or with corpus luteum cyst with intracystic bleeding, thickened cyst wall with fire ring sign (no sign of separation from ovary),...
4.3 When seeing the following images, it can be seen in ectopic pregnancy, it is necessary to coordinate with clinical and β-hCG test to diagnose
No pregnancy in the uterus, or fluid in the uterus (false amniotic sac).
4.4 When ultrasound only shows fluid in the abdomen or pelvis with moderate to large amount, it should be combined with clinical and β-hCG test to make a diagnosis.
Other points to pay attention to
With fluid in the abdomen and pelvis: occurs in about 50-75% in ectopic pregnancy, in about 20% of normal pregnancies in the uterus. Therefore, seeing fluid does not mean that the ectopic pregnancy is ruptured. Ultrasonography can assess intra-abdominal and pelvic fluid as hematopoietic with hyperechoicity, or clot, but has low sensitivity and specificity. Therefore, ultrasound is important to assess whether there is fluid, moderate or high. About 35% of ectopic pregnancies do not show any abnormality on ultrasound at the time of examination (especially those in other sites such as the abdomen). This case requires clinical cooperation, β-hCG testing, even endoscopy and monitoring to diagnose. For other ectopic pregnancy sites: + Interstitial pregnancy: the gestational sac is located at the angle of the uterus with signs of interstitial lines and the uterine lining around the gestational sac < 5mm.
+ Ectopic pregnancy in the ovary: when a yolk sac or embryo is present, the diagnosis is an ectopic pregnancy, when it is only a mixed negative mass, often without signs separate from the ovary, it must be based on clinical, β-hCG testing, even diagnostic endoscopy.
+ Intra-abdominal ectopic pregnancy: often difficult to diagnose. In this case, the ultrasound will not show the pregnancy in the uterus, the ectopic pregnancy will not be seen in the bilateral appendages, it may be necessary to use CT to find the pregnancy mass. Abdominal or pelvic fluid may be seen. In some cases, a pregnancy mass can be seen under the liver....
Understanding the need for reproductive health checks, Vinmec International General Hospital is currently implementing Reproductive Health Checkup Packages. Basic and advanced pre-marriage. In addition, at Vinmec, there is also Vinmec Fertility Center, which is the leading modern center in Vietnam, built and applied a treatment process that combines comprehensive examination, combining both male and female obstetrics and gynecology. to provide the optimal solution for each customer case.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Lin E.P., Bhatt S., and Dogra V.S. (2008). Diagnostic Clues to Ectopic Pregnancy. RadioGraphics , 28 ( 6 ), 1661–1671. Lozeau A.-M. (2005). Diagnosis and Management of Ectopic Pregnancy. Ectopic Pregnancy , 72 (9 ), 8. Williams P.L., Laifer-Narin S.L., and Ragavendra N. (2003). US of abnormal uterine bleeding. Radiogr Rev Publ Radiol Soc N Am Inc , 23 ( 3 ), 703–718. NICE (2019). Recommendations | Ectopic pregnancy and miscarriage: diagnosis and initial management | Guidance | NICE.