This is an automatically translated article.
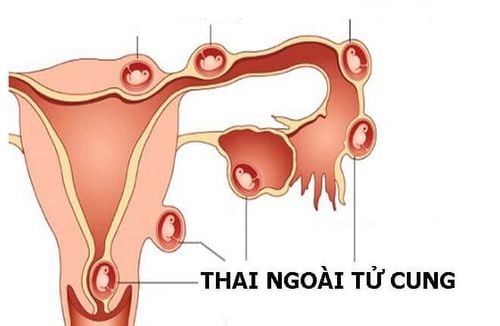
1. What is an ectopic pregnancy?
An ectopic pregnancy occurs when a fertilized egg implants somewhere outside of the uterus, either in the fallopian tubes (fallopian tubes), in the abdomen, or in the cervix. Tubal ectopic pregnancy is the most common because there is a period of implantation of the embryo in the fallopian tube.Although ectopic pregnancy is common, an ectopic pregnancy can also implant in the cervix, ovaries, or anywhere else in the abdomen.
An ectopic pregnancy cannot develop into a normal (non-viable) pregnancy. If left untreated, the fallopian tubes can rupture and cause severe blood loss, which can be life-threatening. Because of these risks, an ectopic pregnancy must be terminated.
An ectopic pregnancy occurs when a fertilized egg implants somewhere outside the uterus (womb). The term tubal pregnancy is also sometimes used, because an ectopic pregnancy implants in one of the fallopian tubes about 95% of the time.
Although it is also known as a tubal pregnancy, an ectopic pregnancy can implant in the cervix, ovaries, or anywhere else in the abdomen.
Non-viable (non-viable) ectopic pregnancy. If left untreated, the fallopian tubes can rupture and cause severe blood loss, which can be life-threatening. Because of these risks, an ectopic pregnancy must be terminated.
2. Value of hCG test in ectopic pregnancy
During pregnancy, your body secretes a hormone called human chorionic gonadotropin (hCG). Low or slowly rising hCG levels can be a sign of an ectopic pregnancy, but looking at hCG levels alone is often not enough for a doctor to make a diagnosis.Asking you to come back to reassess hCG two days later is the best way to track the rate of change. In addition, your doctor may also check your estrogen and progesterone levels to make sure that other hormones that could signal an abnormal pregnancy are not problematic.
While a slow or low rise in hCG levels can indicate an ectopic pregnancy, it doesn't mean you're definitely experiencing one. There are other reasons why hCG levels rise slowly.
There are situations where the following occurs. If you only have a low hCG level, you may be pregnant very soon. Predicting an ectopic pregnancy is easier when your doctor can compare at least two hCG measurements taken over two or three days. This allows the doctor to see if hCG levels are rising and, if so, how quickly.
If hCG levels tend to rise more slowly in the middle and end of the first trimester. If you've had at least two tests for your hCG levels and the hormone doesn't double every two to three days, it can still be considered normal if it's because you're pregnant. 2nd or 3rd trimester.
Your hCG levels will stop rising and start dropping if you have a miscarriage. If you have vaginal bleeding or cramping, or if you notice a loss of pregnancy symptoms (such as breast tenderness, fatigue, and morning sickness), you may be having a miscarriage, not an ectopic pregnancy. bow.
If your doctor thinks you have an ectopic pregnancy, they will usually do an ultrasound (ultrasound). An imaging test that uses high-frequency sound waves to see the inside of your uterus. If no gestational sac appears inside the uterus around the fifth week of pregnancy, it is a sign of an ectopic pregnancy.
Your doctor may also need a pelvic exam to feel for masses in your fallopian tubes and to see if you have pain or muscle tension in your pelvic organs.
If you are diagnosed with an ectopic pregnancy, your doctor may use injections or minimally invasive surgery to terminate the pregnancy. If you are concerned about your future fertility, know that the possibility of pregnancy after an ectopic pregnancy is possible.
Xét nghiệm progesterone khi mang thai giúp đánh giá thai ngoài tử cung giai đoạn sớm
3. Progesterone test in ectopic pregnancy
Progesterone is a steroid hormone produced during the normal menstrual cycle and also during pregnancy. Serum progesterone helps to assess viability of the corpus luteum. During pregnancy, progesterone levels increase gradually and change very little during the first 8-10 weeks.Progesterone has an important role in the evaluation of early ectopic pregnancy. The value of progesterone can help rule out an ectopic pregnancy. The fetus cannot live if the Progesterone level is < 3.5 ng/ml. In this case, it is possible to identify a miscarriage without knowing the location of the fetus. A curettage may be performed for further diagnosis.
According to the author Stern, with an initial progesterone concentration < 5 ng/ml, it can help differentiate between ectopic and intrauterine pregnancy at 4 weeks gestation with 100% specificity and sensitivity. Similarly, at 5 weeks' gestation, the progesterone concentration was <10 ng/ml, at 6 weeks' gestation, the progesterone level was <20 ng/ml but the sensitivity and specificity decreased. When the progesterone level is >25 ng/ml, it is possible to diagnose a normal pregnancy up to 98%. The probability of the patient having an ectopic pregnancy is only about 1.5%.
Thus, if progesterone is <5 ng/ml, it can be diagnosed as an abnormal pregnancy, possibly ectopic pregnancy, incomplete miscarriage or premature stillbirth. With progesterone threshold < 5 ng/ml, the ability to detect ectopic pregnancy early with sensitivity 91.5%, specificity 89.3% positive predictive value 96.2% and negative predictive value 78.1%. 100% of ectopic pregnancies had progesterone levels < 15 ng/ml.
Need to combine with βHCG quantification and fetal ultrasound. The combination of quantitative βHCG and progesterone is considered as a standard to diagnose ectopic pregnancy. When progesterone >12ng/ml, βhCG <2000 UI/L, 80% of pregnancy is normal. In addition, progesterone levels can help differentiate between ruptured ectopic pregnancy and intrauterine pregnancy when β HCG levels suggest pregnancy but a gestational sac has not been detected on ultrasound (in early pregnancy). . With a progesterone concentration >11 ng/ml, an intrauterine pregnancy can be diagnosed with a sensitivity of 91% and a specificity of 84% when ultrasound has not shown a gestational sac.
When conducting a study on 3647 patients who were measured progesterone only once Mc.Cord found that a progesterone concentration ≥ 17.5 ng/ml could allow exclusion of an ectopic pregnancy without the need for any use. another type of test.
Xét nghiệm progesterone khi mang thai có thể chẩn đoán thai ngoài tử cung vỡ và thai trong tử cung
To avoid having an ectopic pregnancy, you should have a screening test before becoming pregnant. This helps you to know your health status, promptly treat and prevent the risk of diseases if any, supplement the necessary nutrients, create the best conditions for the fetus to develop right from the time of birth. Preparing for pregnancy, helping to identify genetic-related risk factors, especially in cases where the parents are suffering from obstetric and gynecological diseases, chronic diseases, have been pregnant or gave birth to a malformed child. natural.
Vinmec International General Hospital is implementing a program of counseling and health care before pregnancy, helping mothers prepare the best health before pregnancy. With this program, you will receive:
General health examination, especially gynecological examination, to help assess the possibility of conception as well as the health of mother and baby during pregnancy. Vaccination before pregnancy, helps prevent many dangerous diseases, especially Rubella. Genetic counseling helps identify risk factors, helps clients and families make decisions, and prevents occurrence or re-emergence in the family. Screening detects healthy people carrying disease genes, especially hemolytic anemia.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.