This is an automatically translated article.
The article is professionally consulted by Master, Doctor Tong Van Hoan - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International Hospital. Doctor with 10 years of experience in the field of Emergency Resuscitation.Pulmonary ventilation is indicated to evaluate the type and degree of pulmonary dysfunction; evaluate symptoms of shortness of breath, cough; early detection of respiratory dysfunction such as interstitial lung disease, chronic obstructive pulmonary disease. Besides, the method of exploratory lung ventilation also evaluates the degree of decrease in lung function for occupational diseases, chronic lung diseases; evaluate the effectiveness of treatment, assess the patient's lung function before surgery...
1. Pulmonary ventilation testing parameters
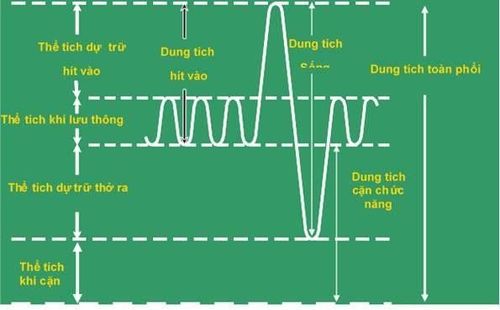
To probe pulmonary ventilation, the patient needs to be measured lung capacities and volumes including: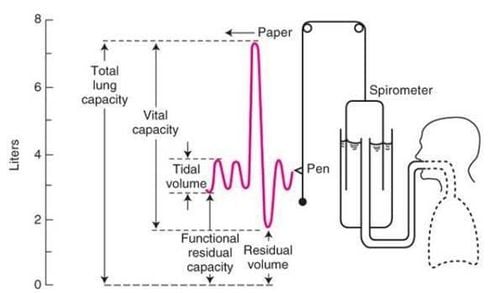
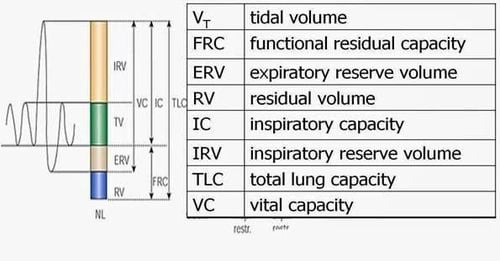
TLC (Total lung capicity): total lung capacity. VC (Vital Capacity): vital capacity. FVC (Forced Vital Capacity): forceful vital capacity. IC (Inspiratory Capacity): Inspiratory capacity. FRC (Functional Ressidual Capacity): functional residual capacity. RV (Residual Volume): volume of residue. ERV (Expiratory Reserve Volume): Expiratory reserve volume. TV (Tidal volume): The circulating volume.
+ Dynamic volumes: are the moving volumes when breathing.
+ Static volumes: are volumes that do not move during breathing.
In which, these volumes and capacities are divided into dynamic volumes that are moving volumes during breathing and static volumes that do not move during breathing.
Pulmonary ventilation probes will include:
Dynamic lung volumes
Vt: Tidal volume is the volume of air that is normally inhaled or exhaled (still breathing). IRV: Inspiratory reserve volume is the amount of air that is inhaled slowly and vigorously after a normal inhalation. ERV: expiratory reserve volume is the amount of air exhaled slowly and forcefully after a normal expiration, which is the result of FRC - RV VC : vital capacity is the forced exhaled volume after a forced inhalation . Static lung volumes
RV: residual volume is the volume of air remaining in the lungs after a slow and forced expiration. Because this is the volume of non-moving gas, so it cannot be measured with a conventional respirometer RV = TLC - VC, if we consider TLC = 100%, the average person RV = 30%. FRC: functional residual capacity is the volume remaining in the embryo after normal expiration. So: FRC = ERV + RV. TLC: Total lung capacity is the volume of air contained in the lungs after maximal inspiration. The current indirect measurement of TLC and RV by three main methods are: Body-volume method is the most accurate method; The gas dilution method uses helium and nitrogen as indicator gases; X-ray method: measured on straight, inclined film from which to calculate TLC and RV, nowadays CT-Scan can be used, but relying on X-ray is the most error-prone method. FEV1 is the patient's forced expiratory volume in the first 1 second then FVC. FEV1 is the basic indicator to diagnose when there is an obstructive ventilation disorder, this indicator has little fluctuation, is easy to measure and is commonly used. Tiffeneau index = FEV1/VC: normal over 75%, this index decreases in obstructive and mixed ventilation disorders. Gaensler Index = FEV1/FVC. This index decreases when below 40% of the theoretical number. FVC mid-maximal flow, or 25%-75% FVC or MMFR segment maximal expiratory flow rate, is the mean expiratory flow rate during mid-life expiratory flow. FEF (25%-75%) is markedly reduced in obstructive ventilation disorders. This indicator has diagnostic value when small airway obstruction. Flow rates at each point in time are evaluated based on: Flow at the site remaining 75% of the volume of the FVC; Remaining site flow 50% volume of FVC; Remaining site flow 25% of the volume of the FVC. These flows are markedly reduced in obstructive ventilation disorders, both in the early stages, but with the disadvantage of high variability between measurements.
Peak flow is the maximum expiratory flow achieved when measuring FVC. PEF is reduced in certain diseases that cause airway obstruction (bronchial asthma, COPD, upper airway obstruction).
2. Some other indicators of pulmonary ventilation testing
Airway resistance is an index of the alveolar-oral difference in flow. Closed volume is the volume of the lung when the airways begin to close. Volume-flow curve: is the relationship between flow and volume from total lung capacity to residual volume. Patients should also know a number of factors that affect the value of the indicators for lung ventilation, such as differences in physical condition, gender, race, environmental factors, smoking, etc. Differences in age, developmental stage, patient's personality, and psychology when performing pulmonary ventilation also affected the values of the parameters.3. The syndromes of pulmonary ventilation disorder
When measuring pulmonary ventilation based on some basic criteria, there will be 4 types of results as follows:3.1. Pulmonary ventilation is normal when: VC >=80%
FEV1 >=80%
Tiffeneau >=75%
3.2. Ventilation disorders restrict VC < 80%
FEV1 normal or decreased
Tiffeneau >= 75%
3.3. Obstructive ventilation normal VC
FEV1 decrease <80%
Tiffeneau decrease <75%
3.4. Mixed dysventilation VC decrease
FEV1 decrease <80%
Tiffeneau decrease <75%
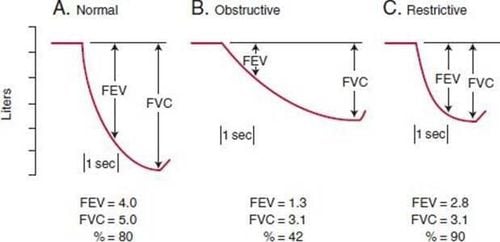
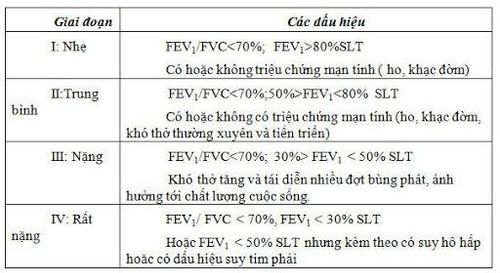
Classification of severity of obstructive ventilation disorder
- Restrictive ventilation disorders due to pleural disease are pleural effusion, pneumothorax of the chest wall: diaphragmatic paralysis, myasthenia gravis, Guillain-Baree, cervical spinal cord injury; chest wall damage: hunchback, obesity...
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














