This is an automatically translated article.
Posted by Master, Doctor Nguyen Van Khanh - Pathologist - Laboratory Department - Vinmec Times City International Hospital
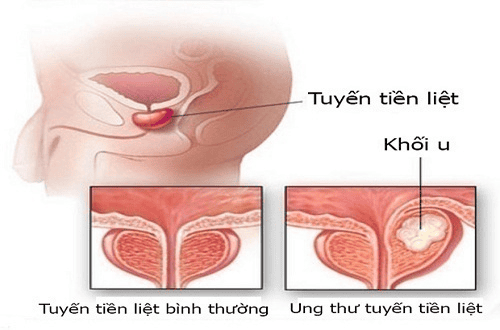
When the prostate is biopsied, the specimen is studied under a microscope by a pathologist, the information in the pathology results will help to accurately assess the disease condition and give directions. treatment. The questions and answers below can help you understand the medical language you often see in the pathology results of a prostate biopsy
1. What does the biopsy result mean by the word “core”?
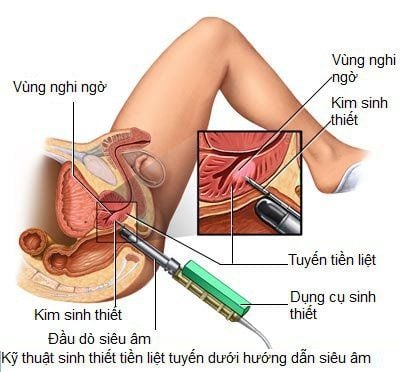
The most common type of prostate biopsy is a core biopsy. For this test, the doctor inserts a thin, hollow needle into the prostate gland. When the needle is withdrawn, a cylindrical piece of prostate tissue called the "core" is removed. This is usually repeated several times to take tissue samples from different areas of the prostate.
The results of your prostate cancer diagnosis as well as your pathology will be listed number by core (or letter), with each core (biopsy) having its own diagnosis. If any cancer or lesions are detected, it's usually not in one core, so you need to look at diagnostics for all cores to know what's going on with you.
2. What is adenocarcinoma?
Adenocarcinoma is a type of cancer that develops from glandular cells. It is the most common type of prostate cancer.
2.1 What is a Gleason Degree or Gleason Score? What do the numbers in the Gleason score, for example 3+4=7 or 3+3=6 mean?
The pathologist grades prostate cancer using numbers 1 to 5 based on the number of cells in the cancerous tissue that look like normal prostate tissue under a microscope. This is called the Gleason system. Grades 1 and 2 are not usually used for biopsies, most biopsy specimens are grade 3 or higher.
If the cancerous tissue looks like normal prostate tissue, it is graded as grade 1. If the cancer cells and their growth components look very abnormal, it is graded as grade 5. Grade 2 for to degree 4 have features lying in between the two degrees above. Because prostate cancer in different regions often has different malignancies, the pathologist will take two degrees in the two areas that make up most of the cancer. These two degrees will be added to form a Gleason score (also known as a Gleason sum). The highest Gleason score is 10 points. The first number is the degree of the most occupied area in the tumor. For example, if the Gleason score is 3+4=7, it means that most tumors have a histological grade of 3 and the area with a grade 4 histology occupies less and these are added together to give a Gleason score of 7. One alternatively this Gleason score could be listed in your results as a Gleason 7/10, a Gleason 7 (3+4), or a combined Gleason grade of 7.
If a tumor has all regions the same grade histology (eg, same grade 3), then the Gleason score is reported as 3+3=6.
Although most Gleason scores are based on the two regions that make up the majority of the tumor, there are exceptions when a core sample either has multiple high-grade cancers or has 3 grades including high-grade cancers. In such cases, the Gleason score is modified to reflect the dangerous nature of the cancer. The higher your Gleason score, the faster your cancer grows and spreads.
2.2 What does a Gleason score of 6, 7, 8, or 9-10 mean?
Because grades 1 and 2 are not usually used for biopsy specimens, the lowest Gleason score for cancer on prostate biopsies is 6. These cancers may be called well differentiated or low grade and they tend to progress and metastasize slowly.
Cancers with a Gleason score of 8 to 10 may be called poorly differentiated or high grade. Cancers are likely to grow and metastasize faster, although a cancer with a Gleason score of 9-10 is twice as likely to progress and metastasize as a cancer with a Gleason score of 8.
Cancers with a Gleason score of 8 Gleason score 7 can be Gleason score 3+4=7 or Gleason score 4+3=7:
Tumors with Gleason score 3+4=7 still have a good prognosis, although it is not as good as tumors have a Gleason score of 6. A tumor with a Gleason score of 4+3=7 is likely to progress and metastasize faster than a tumor with a Gleason score of 3+4=7, but not as much as a tumor with a Gleason score of 8.
2.3 What does it mean for different core biopsy specimens to have different Gleason scores?
Cores can be samples taken from different regions of the same tumor or different tumors in the prostate. Because histology can vary within the same tumor or between different tumors, different cores taken from your prostate may have different Gleason scores. Typically, the highest Gleason score (maximum digit) will be a parameter used by your doctor to predict your prognosis and decide on your treatments.
2.4 Does the Gleason score on a biopsy really indicate the extent of cancer in the entire prostate?
Because prostate biopsies are samples taken from different parts of the prostate gland, the Gleason score on the biopsy often reflects the true extent of your cancer. However, about 1 in 5 cases has a biopsied histology that is lower than the true histology, because the biopsy misses a higher grade (more malignant) cancer. It is also possible that the true histology of the tumor after surgery is lower than the histology on the biopsy.
In the treatment of prostate cancer, currently Vinmec International General Hospital has applied robotic laparoscopic surgery technology in treatment, thereby being able to access narrow and deep terrains, helping overcome the limitations of classical laparoscopy to bring high efficiency in the treatment of prostate cancer. The hospital is one of the leading medical facilities in the treatment of diseases related to the urinary tract. With a system of modern machinery and equipment, a team of doctors and experts with many years of experience will directly participate in the examination and treatment process to bring the most positive results in terms of health for patients. patient.
2.5 How important is the Gleason Score?
The Gleason score is a very important parameter in predicting the progression of prostate cancer and determining the best treatment. Some other information is also important, for example:
Blood PSA level Signs on rectal exam Signs on diagnostic imaging Number of cores containing cancer Cancer is present on either side of the prostate whether the cancer has spread beyond the prostate gland?

3. What are the histological grade groups?
Histological grades are a new way of grading prostate cancer to address some of the problems with the Gleason grading system. As noted above, the lowest Gleason score in practice today is 6, although the theoretical Gleason score ranges from 2 to 10. This leads some patients to think their cancer is on biopsy. is in the middle of the scale. This can make them more anxious about their diagnosis and make them feel that they need immediate treatment.
Another problem with the Gleason grading system is that the Gleason score is usually only divided into 3 groups (6, 7 and 8-10). This is incorrect, because the Gleason score of 7 is made up of two degrees (3+4=7 and 4+3=7), with 4+3=7 having a worse prognosis. Similarly, a Gleason score of 9 or 10 has a worse prognosis than a Gleason score of 8.
To account for this difference, histology grades range from 1 (most favorable prognosis) to 5 (least favorable prognosis) ):
Histology grade 1 = Gleason 6 (or less) Histology grade 2 = Gleason 3+4=7 Histology grade 3 = Gleason 4+3=7 Histology grade 4 = Gleason 8 Grade group histology 5 = Gleason 9-10 Although the histological grade system may eventually replace the Gleason system, the two systems are currently reported side-by-side.
What does this mean if your biopsy results refer to special tests such as high molecular weight cytokeratin (HMWCK), ck903, ck5/6, p63, p40, AMACR (racemase), 34BE12, PIN4 cocktail, or ERG? These are special tests that pathologists sometimes use to help diagnose prostate cancer. Not all patients need these tests. Whether or not the c result refers to these tests does not affect the accuracy of the diagnosis.
4. What do biopsy results refer to perineural infiltrates?
Pericranial infiltration means that cancer cells are found surrounding or running along nerve fibers inside the prostate. When seen on a biopsy, it means the cancer has spread beyond the prostate gland. However, perineural infiltration does not mean that the cancer has spread and other factors are more important, such as the Gleason score and the amount of cancer in the cores. In some cases, signs of perinerveal infiltration can interfere with treatment, so if your report mentions perinerveal infiltration you should discuss it with your doctor.
5. If in addition to cancer, what does the biopsy result refer to high-grade intraepithelial neoplasia or high-grade PIN?
High-grade intraepithelial neoplasia (elevated PIN) is a precancerous lesion of the prostate gland, it is not important in people who already have prostate cancer. In this case, the term "elevation" refers to the PIN and not the cancer, so it has nothing to do with your Gleason score or how aggressive your cancer is.
6. Does the biopsy result refer to acute inflammation (acute prostatitis) or chronic inflammation (chronic prostatitis)?
Most biopsies of inflammatory prostatitis reported on biopsies are not due to infection and do not require treatment. In some cases, inflammation can raise your PAS levels, but it's not linked to prostate cancer. The presence of prostatitis on biopsies of people who have had prostate cancer does not affect their prognosis or their cancer treatment.
7. Does the biopsy refer to atrophy, gland disease, or atypical adenoma hyperplasia?
All of these lesions are benign (non-cancerous) lesions that the pathologist can see under the microscope, but sometimes they look like cancer.
Atrophy is the term used to describe the shrinking of prostate tissue (when it is observed under a microscope). When it affects the entire prostate gland it is called diffuse atrophy. This is usually due to hormones or radiation therapy to the prostate. When atrophy affects only certain areas of the prostate, it is called focal atrophy. Focal atrophy can sometimes look like prostate cancer under the microscope.
Atypical adenomatous hyperplasia sometimes called adenopathy is another benign disease that is sometimes observed on prostate biopsies. It is not important to find any of these lesions if the biopsy also shows prostate cancer.
8. What do biopsy results refer to seminal vesicles mean?
The seminal vesicles are glands located just behind the prostate gland. Sometimes a portion of the seminal vesicle is removed during a biopsy. This is not a cause for concern.
What does this mean if, in addition to cancer, your biopsy results also show atypical glands, atypical small vesicles, atypical adenomas, or atypical hyperplasia? When the pathologist looks at these lesions under the microscope, it is very likely that there is a cancerous lesion somewhere, but not 100% of the cases, it is cancerous. If prostate cancer is already present, these lesions are not important.
In case if your doctor orders special molecular tests to be done on the biopsy sample then these tests can help predict your prostate cancer prognosis and the results should be discussed with your doctor. The results of these tests do not affect the diagnosis, although they may influence the choice of treatment.
The above are considered important explanations for the results of prostate cancer surgery. Hope can bring useful knowledge to help you better understand the current medical condition.
Vinmec International General Hospital with the most advanced equipment, a team of top doctors with many years of experience in the field of oncology and urology is the perfect healthcare address for you and your loved ones. Therefore, when you have health problems, you can go to the hospital to be examined by a doctor and advise on the most appropriate treatment for each medical condition.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Source: American Cancer Society