This is an automatically translated article.
The article was professionally consulted by Dr. Nguyen Anh Tu - Doctor of Obstetric Ultrasound - Prenatal Diagnosis - Obstetrics Department - Vinmec Hai Phong International General Hospital.Peritonitis after obstetric surgery is one of the serious infectious complications after surgery, if not treated promptly, can cause sepsis and other organs leading to death.
1. Peritonitis after obstetric surgery
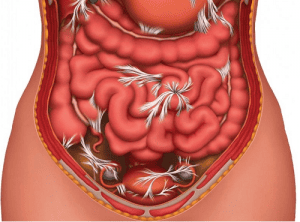
Peritonitis is an inflammation of the thin layer of tissue that covers the inside of the abdomen and most of the internal organs. Accordingly, peritonitis is classified into 3 types:
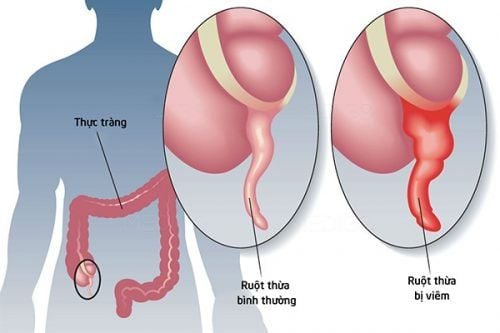
Primary peritonitis: No organ damage, caused by bacteria from the bloodstream or digestive tract into the abdomen without an obvious source. Patients with cirrhosis and ascites have about 10-30% of primary peritonitis and a mortality rate of about 25%. Secondary peritonitis: The result of inflammation of internal organs such as appendicitis, pouchitis. excess , with or without perforation of viscera, infectious complications of abdominal surgery, obstetrics and gynecological surgery (peritonitis after gynecological surgery),... and needing surgical treatment Recurrent peritonitis: Recurrence Infection after adequate treatment of peritonitis is common in patients with comorbidities or immunocompromised patients. In obstetrics and gynecology, two common types are secondary peritonitis and recurrent peritonitis. In addition, if the classification is based on the extent of postpartum infection, there are 2 types of peritonitis: pelvic peritonitis and general peritonitis. In which, pelvic peritonitis is inflammation that is not localized to the uterine lining but develops into the uterus and forms pseudomembranous tissues in the visceral organs, causing adhesions.
2. Causes of peritonitis
There are many causes of peritonitis after obstetric surgery such as:
Bacterial peritonitis: Anaerobic bacteria are Bacteroides, Clostridia and aerobic bacteria include: Lactobacillus, E.coli, Enterococcus , Streptococcus, Staphylococcus, Diphteroides. Postoperative peritonitis secondary to intraoperative infection, cesarean section infection, post-vaginal removal, uterine control, hysterectomy, injury to bladder, ureters, intestines, spread of bacteria overflow from pustular stasis,... Recurrent peritonitis is usually caused by Enterobacter, Enterococcus, Pseudomonas, Staphylococcus and Candida Bacterial peritonitis after pelvic surgery is often caused by many bacteria, 60% are bacteria anaerobes, 20% are Gram (+) aerobic cocci and 20% are Gram (-) aerobic bacilli. Infection in the first 24 hours after surgery is usually caused by Gram (+) cocci, sometimes by Gram bacillus ( -) Infection after the first 48 hours is usually caused by anaerobic bacteria. In addition, risk factors for peritonitis after obstetric surgery such as:
Complicated surgery, long operative time, risk of infection doubling every hour of surgery, even in the case of wound clean surgery Surgery with a lot of blood loss, hematoma and many necrotic tissues Antibiotic failure prophylaxis Surgery in the operating room for infection, emergency surgery for infection doubled
3. What are the symptoms of peritonitis?
Symptoms of peritonitis after obstetric surgery include:
Tachycardia, fever over 38 degrees Celsius, rapid shallow breathing, and low blood pressure Tremors, cold limbs, pale skin, sunken eyes, and fatigue Abdominal distention, abdominal pain, nausea and vomiting Watery stools, or constipation, sometimes unable to pass, and unpleasant odors Anorexia, thirst, little urine, dry skin, dry lips, Decreased skin elasticity due to dehydration and electrolytes Severe symptoms: lethargy and semi-coma. Peritonitis after obstetric surgery, if not treated promptly, can spread rapidly into the bloodstream, causing sepsis and other organs, causing multi-organ failure leading to death.
4. Treatment of peritonitis after obstetric surgery
Treatment of peritonitis after obstetric surgery will become simple if detected early and timely.
4.1 Principles of treatment of peritonitis
Active resuscitation Use broad-spectrum antibiotics, and in combination with multiple antibiotics Emergency surgery to remove infection, wash abdomen and drain.
4.2 Active resuscitation
Intubation of the stomach to reduce intestinal distention Give oxygen if the patient finds it difficult to breathe Rehydrate and electrolytes, avoid secondary systemic disorders For secondary peritonitis, the first day of infusion Albumin 1.5g/kg, after then 1g/kg infusion on the 3rd day to prevent hepatorenal syndrome. Monitor urine output by inserting a Foley catheter.
4.3 Use of antibiotics
Use broad-spectrum antibiotics and a combination of antibiotics as soon as infection is suspected, peritoneal fluid has polymorphonuclear leukocytes ≥ 250/mm3. Adjust antibiotics according to the results of the antibiogram.
Secondary peritonitis: Use antibiotics to cover gram-negative anaerobes, aerobic and other opportunistic bacteria
Possible antibiotics include: Cefotaxime, Ceftriaxon, Ampicillin-sulbactam, Quinolones (Norfloxacin, Ofloxacin, Ciprofloxacin), Metronidazole, Cefotetan, Ticarcillin-Clavulanate, Piperacillin-Tazobactam, Ampicillin-Sulbactam, Imipenem,... with the dose prescribed by the doctor.

4.4 Surgery
Urgent laparotomy: Clear the infection site, then rinse the abdomen and drain. Attention should be paid to the hepatosplenic spaces to avoid residual abscesses. If post-obstetric peritonitis is caused by an infection of the uterine incision, care should be taken when deciding to preserve it because of the risk of recurrent peritonitis. high. After the surgery, the patient needs to be maintained and cared for with a reasonable diet, whereby the patient needs to fast, drink and will be fed intravenously, balancing electrolytes. Feed the patient after bowel movements or when defecating, drain ≥ 4 days after surgery.
In order to prevent peritonitis after obstetric surgery, it is necessary to:
Prepare the patient well before surgery, and complete aseptic procedures Use prophylactic antibiotics in obstetric and gynecological surgeries During in cases of difficult surgery, adhesions, and ascites fluid from before surgery, heavy bleeding, and difficulty in hemostasis,... should place drainage of the cutting apex or through the pelvic cavity During surgery, caution should be taken. when using electrocautery because damage can occur 1-2 weeks after surgery. Monitor symptoms after surgery, pay attention to symptoms such as abdominal pain, fever. For cases after cesarean section, it is necessary to closely monitor the recovery of the uterus, the color and smell of the discharge. In case of infection, when there is a smell of discharge, it is necessary to curettage and give uterine contractions to avoid stagnation of fluid, reduce the risk of surgical incision and peritonitis. For cases of hysterectomy, if there is a fever after surgery, it is necessary to carefully check for blood in the vaginal apex. If in doubt, it is best to examine with ultrasound and remove the apex on the 3rd postoperative day to drain blood and fluid stasis, to prevent infection from spreading and causing peritonitis. Peritonitis after obstetric surgery is a dangerous complication that needs to be handled as soon as possible. Therefore, when the patient has signs of peritonitis, the patient should immediately go to the hospital for examination and appropriate treatment plan.
Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical doctors, modern equipment and technology, but also stands out for its examination and consultation services. comprehensive and professional medical consultation and treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.