This is an automatically translated article.
Pelvic inflammatory disease (PID) is an acute infection of the female upper genital tract, including the cervix, uterine body, fallopian tubes, ovaries, and nearby organs. Most of these conditions are caused by an infection that spreads from the vagina or cervix to the pelvic genitals. If left untreated, pelvic inflammatory disease can lead to serious complications. If you suspect pelvic inflammatory disease, see your doctor as soon as possible.1. Common pathogens.
Chlamydia trachomatis and gonorrhea are the two most common sexually transmitted bacteria associated with pelvic inflammatory disease. Recent studies show that the rate of cases due to Chlamydia trachomatis and gonorrhea is decreasing; In women diagnosed with acute pelvic inflammatory disease, a positive test for either organism is <50%. In addition, Mycoplasma genitalium is believed to be the growing cause. Other bacteria can be encountered under conditions such as aerobic group (Colibacile, Lactobacile, Proteus) or anaerobic group such as (Bactorides, Fragilis, Clostridium). Given the fact that most cases of pelvic inflammatory disease are caused by a variety of bacteria, it can be difficult for doctors to pinpoint the cause, making treatment difficult. Because of the multifactorial nature of the disease, treatment is often the choice of broad-spectrum antibiotic regimens.2. Risk factors for pelvic inflammatory disease.
The disease can occur at any age, more commonly in women < 35 years old; Rarely occurs before the first menstrual period, after menopause and during pregnancy. Women are more likely to get pelvic inflammatory disease if they:Have an untreated sexually transmitted infection, usually due to gonorrhea or Chlamydia trachomatis. Having multiple sex partners, the more sexual partners, the greater the risk. Their partners have sex with other people. Do not use condoms during sex. Previously had pelvic inflammatory disease. Douching can make it easier for the bacteria that cause pelvic inflammatory disease to grow. It pushes bacteria up the uterus and fallopian tubes from the vagina. So douching is not recommended. Use an IUD to prevent pregnancy. It increases the risk about 2 to 3 times during the first 4 months after the ring is inserted, after which the risk gradually decreases. A follow-up visit is recommended within the first month after the IUD is inserted. Women who are not sexually active or who have had a total hysterectomy have very low rates of upper genital tract infections. Bilateral tubal ligation does not completely prevent pelvic inflammatory disease; however, they may have a milder form of the disease.

Đặt vòng tránh thai có thể làm tăng nguy cơ bị viêm vùng chậu
4. Symptoms of pelvic inflammatory disease.
Diagnosis is usually based on a combination of history, physical examination, and other laboratory findings. Women may not realize they have pelvic inflammatory disease because of mild symptoms or no symptoms at all. Because the symptoms are vague, many cases go unrecognized by the woman or the gynecologist.Here are the most common symptoms:
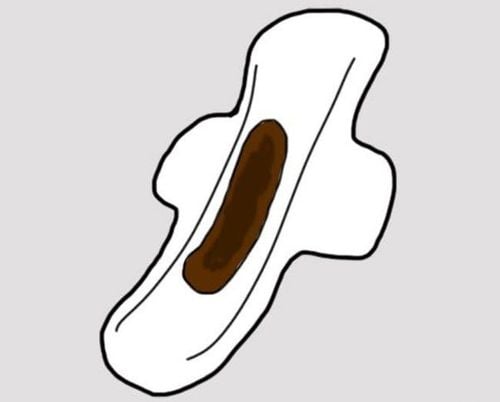
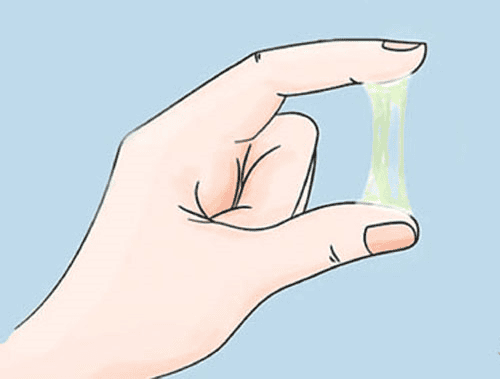
Pain, heaviness, dullness in the lower abdomen, pain that worsens when walking or exercising (this is the most common symptom). Pain or bleeding during and after sex. Bleeding can be irregular bleeding before and after menstruation and menorrhagia. Unusual, foul-smelling vaginal discharge. Dysmenorrhea. Fever (usually just chills). Painful urination, painful urination, frequent urination. If diagnosed and treated early, complications of pelvic inflammatory disease can be prevented. Some of the complications of the disease are:
Formation of scar tissue both inside and outside the fallopian tubes, which can block the fallopian tubes. Ectopic pregnancy (GEU). Infertility. Long-term abdominal/pelvic pain. FITZ – HUGH – CURTIS (Perihepatic Adhesitis)
5. Treatment of pelvic inflammatory disease
5.1 Principles of Treatment All regimens used for treatment must include broad-spectrum antibiotics that are effective against gonorrhea and Chlamydia trachomatis because a negative test for these organisms does not rule out pelvic inflammatory disease. The pathogenic role of anaerobic bacteria in women with pelvic inflammatory disease has not been definitively determined.Treatment should be initiated as soon as the diagnosis is in doubt, as the prevention of long-term sequelae depends on early administration of appropriate antibiotics.
When choosing a treatment regimen, physicians should consider availability, cost, and patient acceptability. In women with mild or moderate clinical severity, injectable and oral regimens were similarly effective.

Cách điều trị viêm vùng chậu phổ biến và hiệu quả là dùng thuốc kháng sinh
A surgical emergency cannot be excluded (eg. , appendicitis ), tubal abscess. Pregnancy. Severe illness. Nausea and vomiting, or high fever. Unable to follow or tolerate an outpatient oral regimen or clinically unresponsive to oral antibiotic therapy. 5.2.2. Intravenous drug therapy Clinical experience will guide decisions regarding conversion to oral therapy, which can usually be initiated within 24-48 hours of clinical improvement. In women with tubal abscess, inpatient monitoring is recommended for at least 24 hours.
Recommended regimens:
Cefotetan 2g IV x 2 times/day (12 hours apart) and Doxycycline 100mg orally or intravenously x 2 times/day (12 hours apart) Or
Cefoxitin 2 IV x 2 times/day (12 hours apart) and Doxycycline 100mg orally or intravenously x 2 times/day (12 hours apart) Or
Clindamycin 900mg IV x 3 times/day (8 hours apart) and Gentamicin injection IV or IM (2 mg/kg), then maintenance dose (1.5 mg/kg) x 3 times/day (8 hours apart). Or use a single daily dose (3-5 mg/kg). Using parenteral Cefotetan or Cefoxitin regimens, doxycycline 100 mg twice daily can be given orally within 24-48 hours after clinical improvement for a full 14-day course of treatment.
For Clindamycin/Gentamicin regimen, oral Clindamycin (450mg orally 4 times a day) or Doxycycline (100 mg x 2 times/day) after stopping intravenous injection for a full course of 14 days.
However, when tubal abscess is present, clindamycin (450 mg orally four times daily) or metronidazole (500 mg twice daily) should be used to complete at least 14 days of treatment with doxycycline to provide coverage. more anaerobic bacteria than Doxycycline alone.
Current research is limited to support the use of other parenteral second- or third-generation cephalosporins (eg, ceftizoxime, cefotaxime, and ceftriaxone). In addition, these Cephalosporins are less active than Cefotetan or Cefoxitin against anaerobic bacteria.
Alternative regimen
Ampicillin/Sulbactam 3g IV x 4 times/day (6 hours apart) and Doxycycline 100mg orally or IV x 2 times/day (12 hours apart) Ampicillin/Sulbactam plus doxycycline has effective against Chlamydia trachomatis, gonorrhea and anaerobes in women with tubal abscess.
5.2.3. Intramuscular or oral therapy Intramuscular/oral therapy may be considered for women with mild to moderately severe acute pelvic inflammatory disease, as clinical outcomes are similar to those treated with pharmacotherapy. intravenous injection.
When patients do not respond within 72 hours should be re-evaluated to confirm the diagnosis and switch to intravenous therapy
Recommended regimens
Ceftriaxone 250mg IM as a single dose and Doxycycline 100mg orally 2 times in 14 days. Whether or not Metronidazole 500 mg orally twice a day for 14 days.
Or
Cefoxitin 2g IM for a single dose and Probenecid 1g for a single dose at the same time and Doxycycline 100mg orally twice a day for 14 days.
Whether or not Metronidazole 500 mg orally twice a day for 14 days.
Or
Other third generation Cephalosporins: Ceftizoxime or Cefotaxime and Doxycycline 100mg orally for 14 days
Whether or not Metronidazole 500 mg orally twice a day for 14 days.
Third generation Cephalsporins are recommended for limited coverage of anaerobic bacteria. Therefore, consider adding Metronidazole to a third-generation cephalosporin regimen.
These regimens offer protection against common causes of pelvic inflammatory disease, but the choice of an optimal cephalosporin is unclear. Cefoxitin, a second-generation cephalosporin, has better anaerobic coverage than ceftriaxone, and in combination with probenecid and doxycycline is effective in the short-term clinical response in women with pelvic inflammatory disease. Ceftriaxone is more resistant to gonorrhea.
Although information regarding other intramuscular and oral regimens is limited, several drugs have undergone at least one clinical trial and demonstrated broad spectrum coverage. Azithromycin demonstrated short-term clinical efficacy in a randomized trial when used as monotherapy (500 mg IV daily for 1-2 doses, followed by 250mg orally daily for 12–14 days ) or in combination with Metronidazole. In another study, it was effective when 1g orally once a week for 2 weeks was used in combination with Ceftriaxone 250mg IM as a single dose. When considering these alternative regimens, the addition of Metronidazole should be considered to include anaerobic bacteria.

Tiêm bắp tay là một trong những cách điều trị viêm vùng chậu cấp tính vừa nhẹ đến trung bình nặng
If the gonorrhea culture is positive, treatment should be based on the antibiotic test results. thing . If the isolate is determined to be Quinolone-resistant gonorrhea or if antibiotic susceptibility cannot be assessed, an infectious disease specialist should be consulted. 5.2.4. Other management considerations To minimize transmission, women should be instructed not to have sex until the full course of treatment has been completed, the symptoms have resolved, and the sexual partner has been treated. full. All women diagnosed with acute pelvic inflammatory disease should be tested for HIV, as well as gonorrhea and Chlamydia.
Monitoring response to treatment Patients usually have clinical improvement (eg, reduced abdominal pain) within 3 days of starting treatment. If no clinical improvement occurs within 72 hours of outpatient intramuscular or oral therapy, hospitalization, evaluation for a change in antibiotic regimen, and additional diagnosis should be made.
All women who have been diagnosed with Chlamydia or gonorrhea should be retested 3 months after treatment, whether or not their sexual partners are treated. If retesting is not possible after 3 months, these women should be retested whenever they visit a health care center for 12 months after treatment.
Management of sexual partners A man who has had sex with a woman with pelvic inflammatory disease in the 60 days before she begins to have symptoms should be evaluated, tested, and treated for Chlamydia and gonorrhea, any Describe the cause isolated from women. If the woman's last sexual contact was > 60 days before the onset of symptoms or diagnosis, the most recent sexual partner should be treated.
Male partners of women with pelvic inflammatory disease caused by Chlamydia trachomatis, gonorrhea, are often asymptomatic. Sexual partners should be instructed to abstain from sex until they and their partners have been adequately treated (that is, until therapy is complete and symptoms have resolved).
5.2.5. Special Cases Allergy, Intolerance and Adverse Reactions Cross-reactivity between penicillins and cephalosporins was <2.5% in individuals with a history of penicillin allergy. The risk of penicillin cross-reactivity was highest with first-generation cephalosporins, but was not significant between most second-generation cephalosporins (Cefoxitin) and all third-generation cephalosporins (Ceftriaxone), and cephalosporins. second generation (Cefoxitin) and all third generation Cephalosporins (Ceftriaxone).
Indication for surgical intervention is not a common indication. Surgical intervention is indicated mainly in cases where medical control cannot be achieved.
Pregnancy Pregnant women with suspected disease have a high risk of preterm delivery. These women should be hospitalized and treated with intravenous antibiotics.
Intrauterine IUD If the IUD user is diagnosed with pelvic inflammatory disease, the IUD does not need to be removed. However, the woman should be treated and closely monitored clinically. If no clinical improvement occurs within 48-72 hours of treatment, removal of the IUD should be considered.

Cho đến khi hoàn thành phác đồ điều trị viêm vùng chậu, phụ nữ được khuyến cáo không nên quan hệ tình dục
6. Reducing the risk of disease by what measures?
Have a healthy lifestyle. Safe sex. Maintain a long-term, mutually monogamous relationship with a partner who has been tested and tested negative for STDs. Do not have anal or oral sex. Use condoms correctly every time you have sex. Get tested for Chlamydia annually if sexually active and 25 years of age or younger. See your doctor promptly if you think you or your sexual partner has or has been exposed to an STD; or you have symptoms that suggest pelvic inflammatory disease. Hygiene during menstruation, personal hygiene and proper intercourse hygiene. Do not douche the vagina. Currently, Vinmec International General Hospital has deployed the Basic Gynecological Examination and Screening Package to help women detect inflammatory diseases early, including pelvic inflammatory disease, and help treat easy, inexpensive. In addition, screening for early detection of gynecological cancer (cervical cancer) is also performed.Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.