This is an automatically translated article.
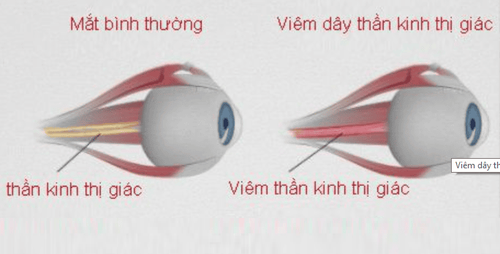
This article is expertly consulted by Master, Doctor Bui Ngoc Phuong Hoa - General Internal Medicine - Department of Medical Examination & Internal Medicine - Vinmec Danang International General Hospital.Optic neuritis is inflammation that damages the optic nerve. Pain and temporary loss of vision in one eye are common symptoms of this condition. The following article provides necessary information about optic neuritis, helping us to recognize the disease from the first symptoms for timely treatment intervention.
1. What is optic neuritis?
The optic nerve is one of 12 pairs of cranial nerves, responsible for transmitting visual signals from the retina (eye) to the occipital lobe in the brain for analysis. Each wire takes on a task for each eye, on a separate market. The two optic nerves have a symmetrical path to both hemispheres of the brain.Optic neuritis is associated with multiple sclerosis (a disease that causes inflammation and damage to many nerves in the brain and spinal cord). Signs and symptoms of optic neuritis may be the first sign of the disease or be acquired later in the course of multiple sclerosis. In addition, optic neuritis can also be the result of other infections or immune diseases, such as systemic lupus erythematosus.
Most people with an episode of optic neuritis eventually recover almost completely. Steroid therapy has been observed to speed vision recovery following this condition.
2. Symptoms of optic neuritis
Optic neuritis usually affects only one independent eye. If the patient has problems in both eyes, the first thing to think about is another condition other than optic neuritis. Symptoms of optic neuritis include:Soreness: Most people with optic neuritis experience moderate to severe eye pain. The pain increases with eye movement. Sometimes the pain is just a vague, dull sensation behind the eye; Loss of vision in one eye: Most patients who go to the doctor are due to a temporary loss of vision of varying degrees. Visual acuity is only markedly reduced when the disease is in an advanced stage, that is, after hours or days. Once the inflammatory lesions are localized, vision improves gradually over weeks to months. However, a small number of cases experience severe vision loss to permanent vision loss; Visual field loss: Unlike visual acuity, the field of vision is the area of space that each eye can see. In optic neuritis, the visual field of one eye is partially narrowed or may be completely absent; Loss of color vision: The ability to perceive color is dependent on the sensitivity of the nerve cells on the retina. And the retina of the eye is also part of the optic nerve. Therefore, the inflammatory response on the optic nerve will also affect color perception. The patient finds that colors appear less vivid than usual or cannot distinguish colors from each other; Flickering light: A small number of patients are found to have optic neuritis when they go to the doctor because they suddenly see flashing lights like lights. The degree of appearance of these images increases gradually or when the patient moves the eyeball. The condition of optic neuritis if left for a long time can progress to more and more serious. In some cases, it can lead to permanent vision loss. Therefore, see your doctor as soon as possible if you notice sudden eye pain or vision changes like the features described above.
In addition, the symptoms of optic neuritis may be accompanied by damage to other nerves, numbness or weakness in one or more limbs, even disturbances of consciousness. At this point, the disease may have progressed seriously.
3. Causes of optic neuritis
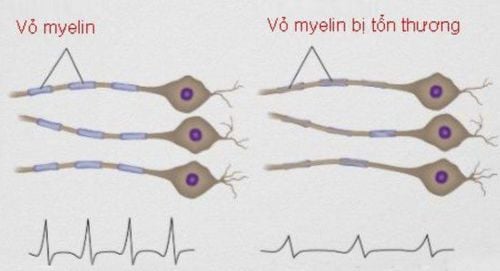
The physiological function of myelins is to help electrical impulses travel rapidly from the eye to the brain, where the stimulus is converted into visual information. Accordingly, the optic neuritis process damages myelin, delays signal transmission, and affects vision.
The following pathologies have been shown to be associated with optic neuritis:
3.1. Multiple sclerosis (MS) Multiple sclerosis is a disease in which the autoimmune system attacks the myelin sheath that covers nerve fibers in the brain and spinal cord. In people with optic neuritis, the lifetime risk of developing multiple sclerosis after an acute episode is about 50%.
The risk of developing multiple sclerosis after optic neuritis is likely to be predicted by magnetic resonance imaging (MRI) of the brain. The more brain lesions that are detected on the MRI, the more severe the presentation will be.
3.2. Infections Bacterial infections, including Lyme disease, cat scratch fever, and syphilis; or viruses, such as measles, mumps, and herpes, can all lead to a complication called optic neuritis.
3.3. Other conditions Diseases such as sarcoidosis and lupus can cause recurrent optic neuritis.
3.4. Medications Some medications can promote optic neuritis, such as quinine and some antibiotics.
4. Risk factors for optic neuritis
Age: Optic neuritis usually occurs in adults aged 20 to 40 years; Gender: Women have been observed to have a higher incidence of optic neuritis than men; Race: In the United States, optic neuritis has been observed to be more common in whites than in blacks; Heredity: Certain genetic mutations may increase susceptibility to triggers that promote optic neuritis or multiple sclerosis.
5. Complications of optic neuritis
Possible complications from optic neuritis include:Optic nerve damage: Most patients have minimal damage to the optic nerve that is permanent after an episode acute inflammation. If the extent of the lesion is large, it can cause clinically significant symptoms; Vision loss: Most patients regain normal or near-normal vision within a few months after the acute episode. However, color confusion symptoms sometimes persist. Many people have permanent vision loss even though the inflammation of the optic nerve has been greatly reduced; Side effects of medications: Steroids are drugs commonly used in the treatment of optic neuritis with the goal of suppressing the immune system. This mechanism creates favorable conditions that make your body more susceptible to infection. In addition, other side effects of steroids include weight gain, osteoporosis, stomach ulcers, gastrointestinal bleeding, impaired glucose tolerance, mood swings, and even addiction. In general, optic neuritis is relatively uncommon in public life, the damage is often localized and has a high potential for recovery; However, sometimes it still leaves serious sequelae. Because the symptoms of this disease are quite typical, it is necessary to actively visit the doctor as soon as there are signs of suspicion of optic neuritis for timely treatment.
Vinmec International General Hospital gathers a team of well-trained and experienced neurologists in the treatment of central nervous system and peripheral nervous system diseases, including optic neuritis. The medical equipment system at Vinmec is modern, meeting international standards, helping to maximize diagnosis and treatment.
Master. Doctor Bui Ngoc Phuong Hoa has more than 24 years of experience in the field of neuropsychology. Doctor Hoa was formerly the Deputy Head of the Department of Neurology - Quang Ngai Provincial General Hospital and participated in many continuous training courses on Epilepsy, Cerebrovascular Accident, Alzheimer's, Movement Disorders, Geriatrics. Endocrine Pathology.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: mayoclinic.org; healthline.com













