This is an automatically translated article.
Article written by Master - Doctor Mai Vien Phuong - Head of Gastrointestinal Endoscopy Unit - Department of Medical Examination and Internal Medicine - Vinmec Central Park International General Hospital.
Bleeding, perforation, and pancreatitis are the most frequent and serious side effects that limit the widespread use of endoscopic papillomatosis. The new laparoscopic papillary resection mentioned in the following article has two main improvements based on conventional methods: One is to isolate bile from pancreatic juice by bile duct stents, the other is to protect the wound surface. with metal clamps and fibrin glue. We will find out more in the article below.
1. Overview of endoscopic papillomaectomy
Tumors of the large duodenal papilla (ball of Vater) are rare, with an incidence of only 0.04% to 0.12% in autopsy studies. Although papillary adenoma (PA) is diagnosed as benign, it has the potential to develop into adenocarcinoma through the adenocarcinoma sequence. Therefore, the treatment of papillary adenomas is necessary and more important than just monitoring.Pancreatic excision and endoscopic papillary resection (EP) are the mainstays of treatment for papillary adenomas. Laparoscopic papillomatosis is more recommended for benign papilloma lesions because of its advantages over open surgery, including less trauma, good outcome, fewer complications, and cost. lower.
With all the above advantages, endoscopic papillomatosis seems to be a promising treatment for papillary adenomas. However, surgeons have also found intraoperative and postoperative adverse events including bleeding, surgery-associated pancreatitis, perforation, cholangitis, papillary stenosis, and some very serious adverse events. critical and even fatal.

A: An endoscopic presentation of duodenal adenoma; B: Submucosal injection; C: A small incision is made when the noose is fixed to a position 0.5 cm from the top edge of the tumor; D, E: The adenoma has been cut with a noose; F: Placement of a pancreatic stent.
2. Difficulty in cutting duodenal lesions
Unlike other gastrointestinal polyps, resection of papillary lesions is much more complicated and difficult for a number of reasons. Such as its complex location in the duodenum, the extremely thick blood vessels and thin wall of the duodenum. Therefore, for a long time, open or minimally invasive surgery, such as pancreaticoduodenectomy, was considered the only removal strategy for papillary adenomas. The limitations of these invasive surgeries are obvious; including adverse event rate, high mortality rate, prolonged anesthesia time, major surgical trauma, high cost,...
3. Endoscopic papillomatosis is valuable in various aspects
Compared with conventional papillomatosis surgery, endoscopic papillomaectomy is valuable in many different respects. The advantages of this method can be mentioned as follows:
(1) For benign lesions, endoscopic papillomaectomy can be a therapeutic approach by completely resecting the lesion with minimal more invasive. (2) For malignancies, endoscopic papillomatosis can provide more tissue for pathological investigations and a defined pathology can guide next step treatments . (3) For patients who are not eligible for prolonged surgery, laparoscopic papillomatosis may reduce the risk of surgery. Although it was first performed in 1987 and has been used by surgeons worldwide, to date there are no standard procedures or guidelines for laparoscopic papillomatosis. Some details, such as pancreatic ductal stenting and submucosal injection, remain controversial.

4. Adverse effects after laparoscopic papillomatectomy
The occurrence of complications after endoscopic papillomatosis is related to two main processes: incomplete healing of surgical cuts and invasion of pathogenic microorganisms. Postoperative adverse events occur in approximately 29% of patients, which is a difficult problem for the endoscopic surgeon and a major cause of death from laparoscopic papillomaectomy in clinical practice. since the widespread adoption of endoscopic papillomatosis. The mortality rate of endoscopic papillomatosis is reported to be about 0.4%. Bleeding and pancreatitis are the most common complications, with reported rates of 4.5% - 45% and 7% - 20%, respectively. Although these complications are uncommon, they limit the wide applicability of endoscopic papillomatosis.Perforation is one of the most serious and dangerous complications of laparoscopic papillomatosis that can lead to severe intra-abdominal infection and even death. Resolving perforation is difficult and often requires the co-operation of liver surgery, which increases surgical risks and costs and reverses the superiority of endoscopic therapy. Therefore, the new method can prevent perforation, making an important contribution to improving the prognosis of endoscopic papillomatosis. In conventional laparoscopic papillary resection, pancreatic ductal stenting is often recommended to relieve postoperative pancreatitis by promoting pancreatic drainage, while the efficacy of pancreatic ductal stents is controversial. Furthermore, the application of common bile duct stents has not been elucidated.
Therefore, a new, better endoscopic papillomaectomy procedure, with fewer complications is required for endoscopic treatment of papilloma lesions. To reduce the postoperative complication rate of laparoscopic papillomatosis and improve the patient's postoperative condition, the authors modified the conventional laparoscopic papillomatosis approach and tested a new procedure. for laparoscopic papillomatectomy in 2016.
5. Modified endoscopic papilloma removal technique by some authors
(1) The patient is placed in the supine position under general anesthesia. (2) Duodenoscopy with a lateral window bronchoscope is used to visualize papillary lesions. (3) A submucosal injection was made to support the lesion; then, a monolithic resection of the lesion was performed. If the lesion is large, partial papillomatosis can be performed; Argon plasma coagulation is used to stop bleeding. (4) A guidewire was used to enter the bile duct (BD) and the guide was retained in the common bile duct. (5) Electrocoagulation forceps and argon plasma coagulation are used to stop the bleeding of the cut and then the cut is closed with metal forceps. (6) A common bile duct stent is inserted. (7) Fibrin glue sprayed into the closed cut. (8) Abdominal free air and stent placement were examined under X-ray. (9) Samples were submitted for histopathology.
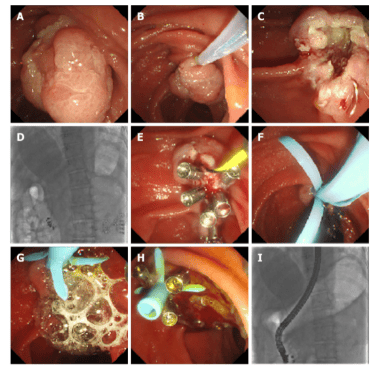
In the new procedure, prompt closure of the cut with metal forceps can help heal the cut and possibly prevent perforation (the most dangerous complication of laparoscopic papillomatosis). It can also prevent bacteria from entering the cut surface or into the ducts.
6. Perspectives on bile duct or pancreatic duct stenting after the procedure
With conventional endoscopic papillary resection, a pancreatic ductal stent is placed simultaneously or with a common bile duct stent, pancreatic juice and bile can escape, cover the cut, and mix. In a mixture of bile and pancreatic juice, bile can activate trypsinogen to trypsin, a substance with strong digestibility. Active trypsin, especially in the pancreatic duct activated by reflux of bile, can cause pancreatitis. It can also induce new granulation tissue on the surface of the cut and inhibit blood clotting, leading to postoperative bleeding.Therefore, the authors suggest that isolating the contact between bile and pancreatic juice might prevent trypsinogen from being activated by bile and possibly reduce the contribution of pancreatic juice to postoperative complications. This new therapy promotes direct bile drainage into the duodenal cavity without covering the cut surface, prevents pancreatic juice and bile from mixing, and does not activate trypsinogen.
In addition, as a protein, the authors suggest that the inactive trypsinogen that coats the cut surface may act as a kind of "nutritional cover" and, together with fibrin glue, may protect and promote healing process. Furthermore, this protective coating can also prevent pathogenic microorganisms from entering the pancreatic duct and may reduce the risk of pancreatitis. Based on these results, the evidence for a new way of endoscopic papillomatosis prevention of postoperative complications is by preventing bleeding and infection of the cut and promoting wound healing.
7. Postoperative treatment and observation
Patient is asked to fast after surgery. Simultaneously, acid secretion inhibitors, enzyme inhibitors (somatostatin) and total parenteral nutrition are also used. Activity-related symptoms, including bleeding, abdominal pain, fever, and postoperative pancreatitis, are monitored closely. The common bile duct stents are removed 3 to 4 weeks after surgery.

8. What does research on new methods say?
The authors performed a single-center, retrospective, comparative study of the new and conventional approach to test the feasibility of the new approach in reducing postoperative complications. A total of 76 patients, of which 23 underwent the new technique and 53 underwent the conventional technique, were retrospectively evaluated in this study. The rate of postoperative bleeding and pancreatitis rate of the new method was significantly lower than that of the conventional method (0 vs 20.75% and 17.4% vs 41.5%).After applying the new method, the most serious complication, perforation, was completely prevented, compared with the rate of 5.66% of the conventional method. Some postoperative symptoms, such as fever, tachycardia, and decreased hemoglobin concentration, were significantly less frequent in the group using the new technique.
Overall, the total adverse complication rate of the new method was lower (0 vs 24.5%) compared with the conventional method. The authors concluded: Patients who underwent the new procedure had lower rates of postoperative complications. This study demonstrates the potential efficacy and safety of the novel laparoscopic papillomaectomy in reducing postoperative complications.
Above is some information about the modified endoscopic papilloma removal method of some authors. Please follow the website: Vinmec.com regularly to update many other useful information.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:Jiang L, Ling-Hu EQ, Chai NL, Li W, Cai FC, Li MY, Guo X, Meng JY, Wang XD, Tang P, Zhu J, Du H, Wang HB. Novel endoscopic papillectomy for reducing adverse events (with videos). World J Gastroenterol 2020; 26(40): 6250-6259 [PMID: 33177797 DOI: 10.3748/wjg.v26.i40.6250]