This is an automatically translated article.
Virus detection techniques are of great help in pathogen identification, although some are only used in research due to their high cost and slow results.1. Overview of pathogenic viruses
Virus is also known as a virus, a virus or a virus. This is an infectious agent that can only multiply inside a living cell of another organism. Viruses can infect many types of organisms, from animals and plants to bacteria and archaea.
Currently, viral diagnostic methods can detect more than 500 viruses capable of causing disease in humans. More and more new viruses are discovered, causing diseases that are global health problems such as HIV, hepatitis B... Viral infections can be acute, chronic, latent or infectious. Infection is slow and can also cause cancer. Among them, acute or chronic viral infections with consequences are the most common.
Viruses that survive in the wild need to continue infecting susceptible individuals. In an infected host, the virus can cause an acute infection or can cause a long period of persistent infection.
In the acute phase of infection, the virus is usually destroyed by the host's immune response. Therefore, some viruses that cause acute infections, such as measles virus, mumps virus, survive by continuously infecting human populations; on the contrary, some other viruses such as influenza virus, yellow fever virus, rabies virus... circulate in nature on another species. But there are still other viruses, which themselves have structural features that allow them to survive for a long time until meeting an infected host.
2. Methods of diagnosing disease-causing viruses
2.1 Rapid Detection by Microscope A microscope is a device used to observe objects so small that the naked eye cannot see them by creating magnified images of the object. Microscopes can increase normal magnification up to 40 - 3000 times.

Kính hiển vi có thể phóng đại bình thường lên từ 40 - 3000 lần hình ảnh vật thể
2.2. Rapid detection by electron microscopy This is one of the methods of virus diagnosis. A reasonable method for virus detection from clinical specimens is applied to detect virus from pus-filled (pox) swabs, fecal (rota) samples, etc. However, if the virus titer is in the test sample low will not be detected by microscopy.
2.3. Antigen detection For viruses that do not have multiple serotypes, direct detection of antigens is a rapid diagnostic method in the laboratory, but the antigen present in the sample must be present in sufficient quantities for serological detection. standard.
2.4. Immunofluorescence and immunoperoxydase staining This method is used to detect upper respiratory tract viruses such as RSV, influenza A and B viruses, parainfluenza viruses types 1, 2, 3, 4a and 4b, mumps virus measles virus. In addition, it can also be used to detect Herpes Simplex virus from vesicles... The success of the technique depends on sample quality and specimen preparation techniques.
2.5. Solid-phase immunoassay Solid-phase immunoassay has many advantages in diagnosing viral diseases such as being very fast - just a few minutes to a day to perform, using clinical specimens at an early stage of the disease, there is very early information for the management of acute cases... Some human diseases have successfully applied solid phase immunoassays in diagnosis, such as hepatitis A and B viruses, Rotavirus, infectious agents. Norwalk virus, Adeno virus, HIV...
2.6. Fluorescent antibody method Fluorescent antibody (FA) method is mainly used to evaluate BAL fluid or fresh/frozen lung tissue, but currently has very little application. In this technique, the sample is directly attached to fluorescent antibodies to view the nucleocapsids.
This process is faster and cheaper than the IHC technique to detect PRRSV but, like IHC, it cannot detect genetically diverse strains of the virus and is not recommended in the later stages of the disease. Furthermore, false positives can be problematic because of the low specificity of the primary antibody or the high background staining. In either case, positive samples should preferably be retested by RT-PCR (or virus isolation).
2.7 Rapid Test Kits Rapid test strips are a relatively new development for PRRSV virus diagnosis, and although not yet widely used, they are useful in fast and convenient PRRS virus detection. without expertise or special equipment.
Hình ảnh virus PRRS
These checkers help detect virus in serum or in tissue fluid by immunochromatography. These samples are mixed with gold-labeled monoclonal antibodies that target specific PRRS proteins, the protein-antibody combinations are stored on test strips. The conjugates held on these bars are detected through a previously attached second antibody.
In studies in China, these test strips have demonstrated sensitivity in excess of 93% and specificity in excess of 96%, however current data are still only on a limited range of viruses .
2.8. Xtag Multiprimer PCR Molecular Technique This is one of the virus diagnostic methods that only help detect individual viruses. The application of the new xTAG PCR technique, which can detect 18 respiratory viruses at the same time, has made the process of detecting and treating respiratory diseases simple, convenient and highly effective.
This method is evaluated as having high sensitivity and specificity, the time to return results is shortened to 24g. The early detection of viral causes of respiratory infections helps to limit unnecessary antibiotic use for patients, improve treatment efficiency and reduce treatment costs.
2.9 Reverse Passive Hemolysis (PHA) As a result of this method, if HBsAg is present in the test serum, agglutination will occur because sheep erythrocytes will passively aggregate.
The reaction is negative when no agglutination occurs, nodular or ring-shaped appearance of unagglutinated red blood cells settle to the bottom of the well. The reaction is positive when agglutination occurs, without buttons or rings.
This method does not need expensive tools, simple to conduct, read results with the naked eye, so it is also widely used to diagnose other diseases. However, it is less sensitive than the ELISA technique.
2.10 Chromatography Immunoassay This test is simple, fast, takes only a few minutes, reads the results with the naked eye. Together with the agglutination technique, the WHO-recommended rapid test technique can be used to screen blood in small laboratories, in remote locations or in emergency situations.
Currently, the HBsAg rapid test is applied to screen blood donors at the volunteer blood donation site, then screen the donated blood unit again by ELISA or chemiluminescence at the laboratory. experience.
2.11 Enzyme-linked immunoassay (ELISA) Known antibodies (or antigens) immobilized on the solid phase, the most commonly used solid phases are:
On the bottom and sides of the plastic wells On the surface of the polystyrene beads or other material On the surface of special, disposable instruments for automated systems. Nitrocellulose solutions or membranes. This method is often used in the Western method.
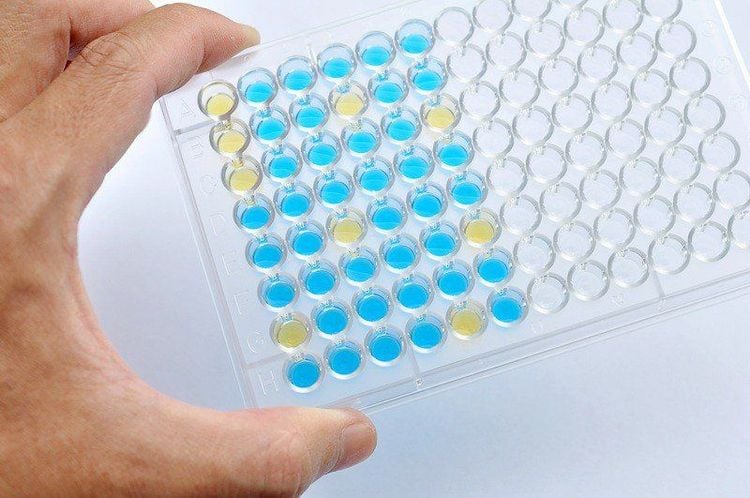
Đĩa ELISA được dùng cho các xét nghiệm miễn dịch liên kết với enzym ELISA là một công cụ chuẩn đoán lâm sàng
The enzyme conjugates with the chromophore system acting as a detection system for the antigen-antibody complex is formed.
2.12 Microparticle Enzyme Immunoassay (MEIA) A recent improved ELISA method using microparticles and microcomputer media provides relatively fast (45 min) microparticle enzyme immunoassays (MEIA) and fully automatic.
The basic principle of the microparticle test, which is different from the well test, is that the entire surface of a gelatin or latex granule is approximately 1 mm in size in suspension with a suitable buffer. Each test uses one volume of suspension, which is composed of millions of tiny particles. These particles provide a large surface area for the reaction. Most microparticle assays are designed for specialized systems and are contained in small wells in which the reaction occurs. The technical principle and method are the same as the ELISA technique. Abbott's PRISM and AxSYM systems are examples of this test.
2.13 Electrochemiluminescence immunoassay (ECLIA) This technique was performed on a fully automated machine.
Use known antibodies to detect unknown antigens, and vice versa. Use an electroluminescent detection system to detect the presence of antigen-antibody complexes.
The technique includes the following reactions:
Immunoassay: antigen-specifically conjugated antibodies labeled with ruthenium. Use the interaction of biotin and streptavidin together with magnetic microparticles to attach the antigen-antibody complex (labelled with ruthenium) to the solid phase. Electroluminescence: to detect the presence of antigen-antibody complexes labeled with ruthenium. Under the action of electricity, the ruthenium complex reacts with tripropylamine (TPA) and fluoresces. The result of the electroluminescence reaction is a light signal that is recorded by the machine and inferred the initial concentration of the antigen or antibody present in the sample.
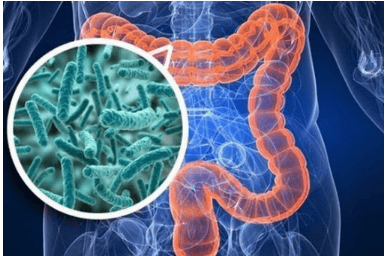
2.14 Serological diagnosis Antibody quantification method: There are following methods to determine anti-viral antibodies: (a) Direct method of determining the interaction between antigen and antibody; (b) Methods that depend on the ability of the antibody to interact with the antigen, performing some non-viral function; (c) Method for the direct determination of the ability of antibodies to interfere with some specific viral function. Antibody response to viral infection: In most primary viral infections, antibodies are significantly elevated in serum. Therefore, determination of antibody levels in a pair of serum samples collected early in the course of the disease (acute) and late or after recovery (remission) can be used to make the diagnosis. However, there are some exceptions where there is no antibody response after viral infection. Quantification of IgM and IgA antibodies: IgM antibodies are usually produced soon after viral infection, usually persisting for 1 to 3 months, sometimes longer. Detectable IgM in many cases means viral replication or presence. Therefore, IgM quantification is an effective tool in viral diagnosis for early diagnosis in the course of infection, very useful for patient management. The IgA antibody is also produced early, but it usually lasts longer than IgM. Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading doctors, modern equipment and technology, but also stands out for its examination and consulting services. and comprehensive, professional medical treatment; civilized, polite, safe and sterile medical examination and treatment space.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.