This is an automatically translated article.
Low birth weight infants are those with birth weight less than 2500g regardless of gestational age. Classification of low birth weight babies divided into 3 groups: Premature babies; Intrauterine growth retardation; Premature infants associated with intrauterine growth retardation.1. Definition and classification of infants
Full-term infants: Those with a gestational age of 37 - 42 weeksPreterm infants (premature babies): Are babies born before term, with a gestational age of less than 37 weeks.
Babies born under 22 weeks are called miscarriages.
Premature babies: Those with a gestational age of more than 42 weeks
Low birth weight (low birth weight): These are babies with birth weight <2500g, regardless of gestational age. Classification of low birth weight babies (according to Luchenco) is divided into 3 groups as follows:
Premature babies: Babies with normal intrauterine development, but births occurring before 37 weeks, with a weight commensurate with gestational age (weight) baby's birth weight is between the 10-90% centile) Intrauterine growth retardation (fetal malnutrition), including full-term, old-term infants but birth weight <2500g Premature babies associated with intrauterine growth retardation (premature infants with fetal malnutrition or preterm infants): These are infants born before 37 weeks of gestation and have a low birth weight <10% percentile (weight lower than gestational age). Real age: The actual age of a premature baby is equal to the age in date of birth minus the difference between the gestational age of a full-term infant and the gestational age at birth. Specifically calculated according to the following formula:
Real age = age by date of birth - (40 weeks - gestational age at birth)
2. Gestational age
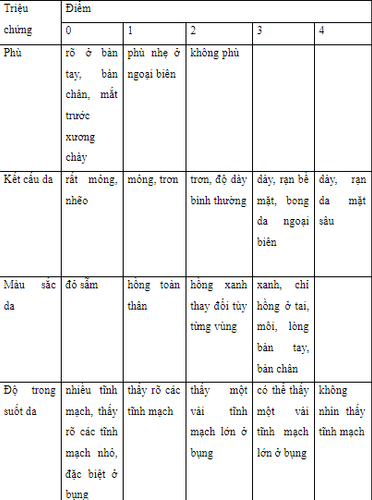
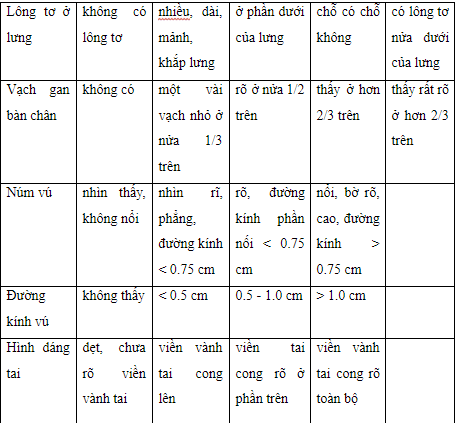
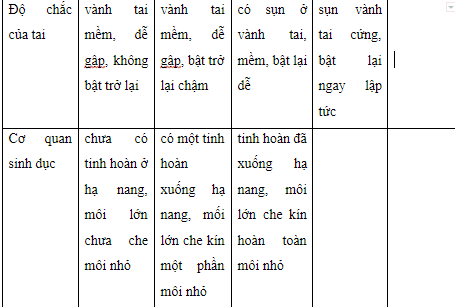
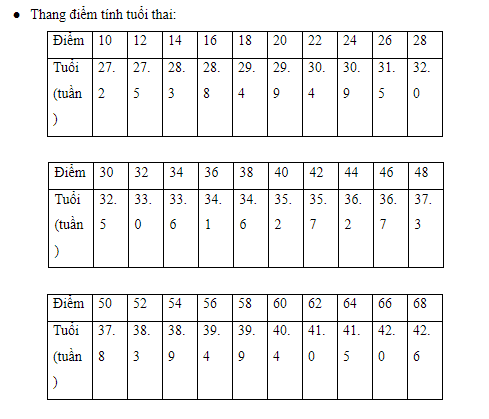
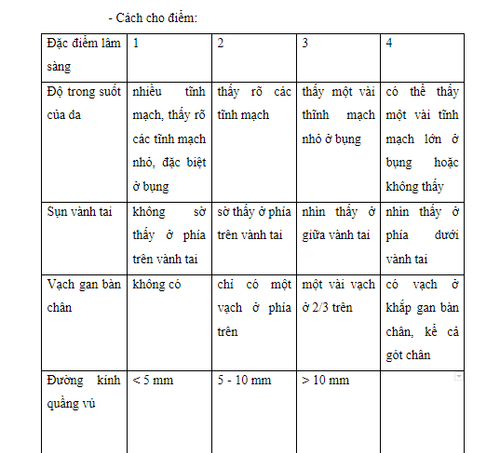
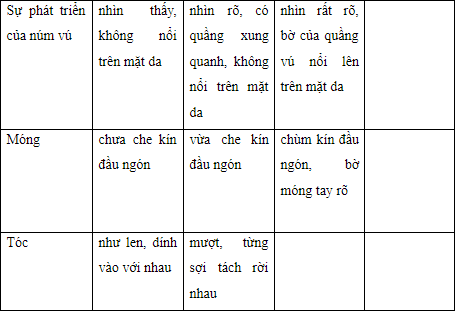
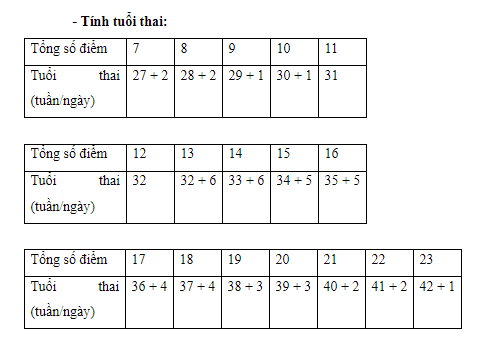
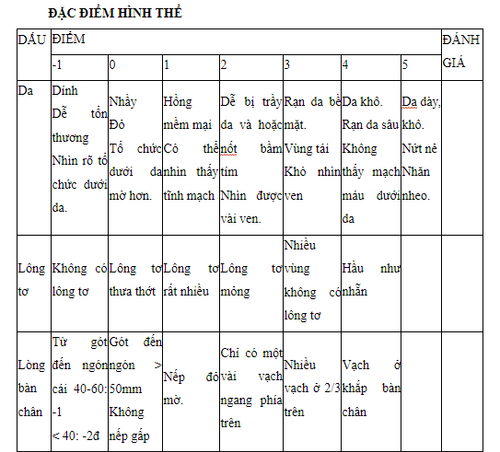
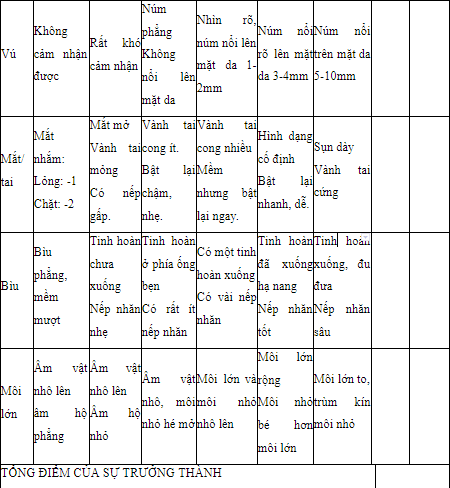
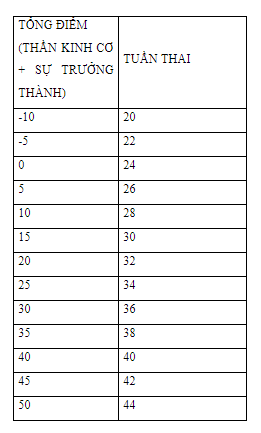
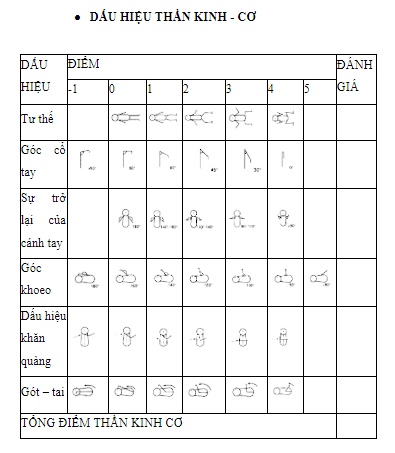
Calculating gestational age There are many ways to calculate gestational age:Method 1: Based on the first day of the last menstrual period. Normally about 280 days (day +10, month -3). Method 2: Based on fetal ultrasound at about 10-12 weeks of age. We can predict the gestational age based on head circumference, head index = biparietal diameter/parietal frontal diameter, chest circumference, femoral length Method 3: Clinical examination after the child is born Classification of gestational age Premature babies are babies with a gestational age < 260 days ie < 37 weeks. A full-term baby is a baby with a gestational age of 260 - 294 days ie 37 - 42 weeks. Premature infants are those with gestational age > 294 days, ie > 42 weeks. Calculation of gestational age based on Dubowitz's scale Based on the total score of physical and nervous system characteristics.
Physical features
3. Causes of children giving birth
3.1 Maternal causes Obstetric and gynecological causes:Uterine malformations, uterine fibroids, ovarian cysts, appendicitis, ... Toxic pregnancy, placenta previa, polyhydramnios, Rh incompatibility. Medical causes:
Chronic diseases: heart, lung, kidney, diabetes,... Infections: pneumonia, flu, hepatitis, listeriose. Surgical causes:
Direct trauma: fall Indirect trauma: surgery during pregnancy. Genitourinary disorders: history of miscarriage, multiple premature births.
3.2 Cause of child Multiple pregnancy, deformity.
30% of cases no cause is found. There are also some favorable factors such as:
The mother is too young (less than 15 years old), too old (over 40 years old). Hard working conditions. Difficult economic conditions, little monitoring of pregnancy.
4. Identifying characteristics of premature babies
Weight at birth is less than 2500g Body length at birth is less than 45cm Skin: The younger the baby, the redder, juicier the skin is, the blood vessels under the skin are clear, the skin has a lot of hair, especially on the shoulders and back. Thin layer of subcutaneous fat Soft muscle, reduced muscle tone, child lying in a position of extensor limbs, little movement. Soft bones, big head to body ratio (1/4), wide fontanel, soft ears, underdeveloped auricular cartilage. Short hair less than 2cm, especially in the top forehead area, curly hair like wool. Fingernails and toenails are soft, not covering the tips of the toes. The external genitalia are not fully developed: in boys, the testicles have not yet descended to the hypocyst; In girls, the big lips have not yet covered the small lips and clitoris. Nervous: The baby is lethargic, unresponsive, crying weakly, newborn reflexes are weak or absent.
Trẻ sinh non có cân nặng lúc đẻ dưới 2500g
5. Common diseases in premature babies
5.1 Hypothermia In infants who cannot yet produce heat by contracting muscles, they can only produce heat by breaking down brown fat tissue. This form of thermogenesis does not adequately compensate for post partum heat loss. As a result, the child increases the consumption of energy, oxygen and glucose, causing a metabolic acidosis due to the release of free fatty acids and lactate. Especially in premature babies, the layer of fat is thin, the insulation is thin, the storage of brown fat is small, while the skin area is large (the ratio of skin area to body weight in full-term neonates is 2.7 times higher than that of adults). , in premature infants less than 1000 g, this rate is 4 times higher than in adults), causing increased heat loss after parturition.Main causes of heat loss:
Convection: depends on the temperature difference between the environment and the child and the air velocity. To limit heat loss through convection, we must: keep the room temperature at least 280C, close the door to prevent air circulation, wrap the child when placed on the emergency table, heat up oxygen. Heat transfer: depends on the temperature difference and the thermal conductivity of the contact object. Heat transfer is increased when using glass tables, metal utensils: film containers. Radiation: caused by cold objects in the environment (windows, ceramics) and depends on the fourth power of the temperature difference. Therefore, we must use a 2-layer incubator, a plastic blanket... Evaporation: mainly lost through the skin and respiratory mucosa. In the postpartum period, every 1 g of water evaporated, resulting in a loss of 0.58 kCal. This phenomenon occurs especially strongly in premature infants less than 32 weeks. Therefore, care must be taken to humidify the air. 5.2 Respiratory failure Respiratory manifestations are common and severe. The disease ranks first in the pathologies in the neonatal department.
Inner membrane disease :
Caused by a lack of sulfactane. Diagnosis is based on respiratory distress syndrome occurring in premature infants under 35 weeks, acute in the first day or second day after birth, symptoms of respiratory muscle contractures are very obvious. Symptoms to confirm the diagnosis are X-ray images: low lung expansion, diffuse opacities in 2 lung fields, decreased brightness of lung parenchyma, air stasis in bronchial branches. Treatment: immediate respiratory aid + surfactan. A common consequence is pulmonary edema, or retinal edema, caused by prolonged and high doses of oxygen. Delayed absorption of alveolar fluid leads to respiratory failure lasting several hours after birth. Common in low birth weight infants.
The respiratory center is incomplete, causing "primary" apneas lasting from a few seconds to 20 seconds. May cause bradycardia and cyanosis if apnea persists.
“Secondary” apnea in the following diseases: cerebral hemorrhage, meningitis, meningitis, hypoglycemia, hypocalcemia.
5.3 Digestive diseases

Cần chú ý rằng trẻ đẻ non ỉa phân xu kéo dài hơn trẻ đủ tháng
Stomach and breast milk deposits: common in babies under 34 weeks. Attention must be paid to evaluate the nature of milk residue before each meal to decide:
Use re-injection into the stomach if the fluid is small, white. Discard if the amount is large, must be fed with a nasogastric tube. Pyloroduodenal stasis syndrome: yellow, green, and abundant gastric stasis, common in neonates weighing less than 1500 g. Indication of parenteral nutrition, or feeding in the small intestine will avoid this complication.
Abdominal distention: due to stagnation in the intestinal loops. Unprepared X-ray showed dilated bowel loops. Pay attention to exclude necrotizing enterocolitis. May be accompanied by symptoms of gastric juice, green stools. Indications for parenteral nutrition for 2-3 days.
Syndrome of "coincidence button": common in premature babies. Clinically, it is common to see slow peritoneal dilation, abdominal distension, and normal general condition.
Unprepared abdominal X-ray shows dilated bowel loops. Colon enema with physiological saline helps the child excrete thick stools.
Necrotizing enterocolitis: often has serious, varied and potentially fatal complications. Accounts for 1-2% of premature babies admitted to the hospital.
Necrotizing inflammation, bleeding, ulceration in the intestine (2/3 of cases in the ileocecal region), with gas infiltration in the submucosa.
Common in the first week postpartum. Clinically, it is common to see yellow or green vomiting, bloody stools, and abdominal distension. The whole body is in a very serious condition, the skin is green, the skin is purple, the child is lethargic, there is a pause in breathing, and the heart rate is slow. Abdominal X-ray unprepared: the typical picture is an air bubble in the intestinal wall. Possible complications are intestinal perforation, peritonitis. Medical treatment is the main treatment, 10% is surgical treatment when there are complications of intestinal perforation, peritonitis. Mortality rate 10 - 25% depending on statistics. 5.4 Anemia Anemia when the Hb concentration is < 13g/dl in children ≥ 28 weeks old and < 12 g/dl in children < 28 weeks old
Clinical symptoms: 50% of infants under 32 weeks show anemia on clinical.
Acute anemia: tachycardia. Tachypnea – shallow, peripheral pulse weak or absent, arterial blood pressure drop, central venous pressure drop, shock, metabolic acidosis. Chronic anemia: pale skin, rapid breathing, tachycardia, normal pulse, hepatosplenomegaly, heart failure, normal arterial blood pressure. Causes:
Bleeding in the fetal period (bleeding placenta, injury during amniocentesis, cesarean section, mother-child blood transfusion, fetal-fetal blood transfusion) and in the neonatal period (ejaculation) cerebral hemorrhage - meningeal, gastrointestinal bleeding, retroperitoneal bleeding, umbilical cord bleeding...) Hemolysis: blood group incompatibility, thalasemie. Take blood for testing many times, especially in children with very low birth weight. Lack of material for red blood cell synthesis in late anemia. Mechanism:
Impaired erythropoietin synthesis in the first weeks postpartum is the main cause of early anemia. Erythropoietin synthesis in relation to venous hypoxia. Immediately after giving birth, the amount of erythropoietin increases and decreases rapidly in the first weeks after parturition, much lower than that of adults, explaining the above phenomenon. But there are a few studies that did not show a decrease in erythropoietine levels, so it has been suggested that the anemia is due to a disorder of the response to erythropoietine. Treatment:
Transfusion of red blood cells in the following cases:
Hematocrit < 40%, Hb < 11g/dl, when the child has respiratory failure and/or heart failure. Hematocrit < 25%, Hb < 8 g/dl, when the child has tachycardia > 180 beats/min, tachypnea > 80 breaths per minute, dependent on oxygen for more than 48 hours. Anemia in premature infants with apnea, abdominal distension, slow weight gain, poor feeding. Blood transfusion when more than 10% of the child's blood volume is taken (about 8 - 9 ml/kg). Hemolytic anemia after 1 week when hemoglobin < 10 g/dl Pay attention to provide iron daily for premature infants from the 2nd week of life at a dose of 2 mg/kg/day in term infants, 2-4 mg/kg per day in premature infants. Vitamin E 15-25 units/day for up to 38 weeks. Erythropoietin is indicated for infants under 30 weeks of age at a dose of 250 units/kg x 3 times/week intravenously or subcutaneously, from the end of the first week postpartum, within 4-6 weeks. 5.5 Neurological complications

Trẻ sinh non có thể sẽ gặp biến chứng thần kinh như xuất huyết não, nhuyễn não chất trắng
Brain hemorrhage: common in the first 3 days of life, may experience antenatal bleeding. Intracerebral hemorrhage on days 5 and 6 is uncommon.
Favorable factors:
All factors deregulate cerebral circulation, increase cerebral perfusion. Increased carbon dioxide in the blood, acidosis leads to dilation of cerebral blood vessels. Cerebral vascular rupture and incomplete coagulation lead to bleeding. Diagnosed by transthoracic ultrasound, cranial CT
The rate of brain hemorrhage is higher in the younger children: 60% of intracerebral hemorrhage occurs in children under 28 weeks.
Ischemic brain injury: leukoencephalopathy leads to long-term neurological consequences.
Common locations: anterior and posterior horns of the lateral ventricles, lateral to the lateral brain stem, anterior and occipital horns. These are areas with few arcuate arteries. In premature infants this area is up to several mm wide. All causes of cerebral ischemia are causes of white matter brain necrosis. Occurs before delivery: toxemia of pregnancy, placenta previa bleeding, placental abruption. Occurs after birth: especially vascular collapse. Diagnosed by transfocal ultrasonography, cranial CT. The location, size, and number of lesions will help predict the future. The incidence of white matter brain necrosis is 12–15% in infants under 1500g, 8% in infants older than 34 weeks. 5.6 Infection Prematurity can be caused by an infection of the membranes, or premature rupture of the membranes causing secondary infection. Postpartum infection in the hospital stay is a concern of neonatologists because the child's resistance is very weak. Common infections at the hospital: gastroenteritis, which can cause necrotizing enterocolitis, lung infection, skin infection... Prevention: wash hands before and after each medical examination, thoroughly disinfect the cage Incubate, cloth, absolutely ensure the principle of sterility when performing procedures, infusion.

Cần rửa tay trước và sau mỗi lần khám để phòng ngừa nhiễm trùng sau sinh cho trẻ
Symptoms of ductus arteriosus are:
Increased respiratory distress (respiratory aid required on day 2). - 5, increased oxygen demand...) Systolic murmur, rarely continuous, may be inaudible. Must check several times a day. The pulse is bouncy and fast. Chest X-ray showed pulmonary edema. Echocardiography clearly shows the ductus arteriosus. Treatment:
Limit fluid intake: Children under 1000g: 100 ml/kg/day; 1001 - 1500 g: 80 ml/kg/day; over 1500g: 60 ml/kg/day If the child is still edematous, furosemide 1mg/kg can be given, reducing fluid intake. Ensure oxygen needs for children. Drugs: Indomethacin to inhibit the prostaglandine system. Prophylactic dose: 0.1 mg/kg/dose intravenously 12, 24, 48 and 72 hours postpartum. Therapeutic dose 0.2 mg/kg/dose x 3 doses 12 hours apart. Slow intravenous injection. Ibuprofene: 10 mg/kg then 5 mg/kg 24 and 48 hours. Intravenous injection. Common complications when using the drug are VRHT, kidney failure, bleeding. If the ductus arteriosus does not close after drug therapy, surgical ligation is performed. 5.8 Metabolic disorders Hypoglycemia: due to increased consumption (to ensure body temperature, maintain respiration), poor glycogen stores. Symptoms varied: shivering, cyanosis, respiratory failure, apnea, abortion, convulsions, hypothermia...). Treatment: 3-4 ml/kg Glucose 10% slow intravenous injection, then infusion with a concentration of 0.3-0.6g/kg/hour. Hyponatremia: <130 mmol/l due to immature tubules, Na loss, hormone deficiency and/or no effect on the tubules. Loss of water into the intercellular space, so the amount of fluid should be limited. Hypocalcemia: < 2 mmol/l due to calcitonin activity, hyperphosphatemia, maternal vitamin D and Ca deficiency during pregnancy. Children often increase arousal, tremor, hypertonia, In severe cases children convulsions, cyanosis, apnea, heart enlargement, tachycardia, QT interval prolongation. Room with calcium 0.3g/kg/day, VTM D 1500 units/day. Treatment is with calcium 1000-1500 units/m2/day intravenously then orally, combined with VTM D. In case of convulsions, slow IV injection of calcium chloride 10-20 mg/kg/day. 5.9 Liver Vitamin K deficiency: reduces prothrombin ratio, risk of bleeding. Prevention by injecting VTM K for all newborns 1-2 mg Jaundice: seen in 60% of premature babies. Caused by glucuronyl transferase deficiency associated with protein reduction, hypoglycemia, enterohepatic cycle. Possible complication is cerebral yellowing. Prevention of complications by monitoring blood bilirubin levels and lighting. 5.10 Retinopathy of prematurity The vessel wall is highly permeable and fragile due to lack of carboxylic esterase enzymes, especially in the absence of oxygen. When blood oxygen is too high (PaO2>150 mmHg) and prolonged, blood vessels in some places such as the optic nerve area, retina may shrink, poor cell nutrition, may cause cell damage. Therefore, when the neonate is mechanically ventilated with high and prolonged oxygen concentration or the premature infant (<1500g) is placed in an incubator with an oxygen concentration >40% for a long time, blindness can result from retinal atrophy. and the back of the vitreous
6. The future of premature babies

Trẻ sinh non cần có sự quan tâm chăm sóc đặc biệt từ phía gia đình cũng như bác sĩ
Neurological complications in premature infants: long-term follow-up is required. During the pre-school period, we encountered the following complications:
Temporary neurological abnormalities: increased excitability, abnormal muscle tone in the back and lower extremities. It can go away at the school stage. Neurological and mental sequelae: paralysis of 2 limbs, quadriplegia, mental retardation, blindness, deafness. Sequelae of cerebral hemorrhage and white matter brain necrosis. Injuries to the forehead have a good prognosis, lesions of the apex often have movement disorders, and the occipital region affects vision. Long-term follow-up:
Neurologic sequelae: as above. During the school period, we can meet children with hyperactivity, increased arousal, and loss of concentration in 24% of premature babies. Difficulty with pronunciation, spatial orientation, coordination and movement. Therefore, premature babies need special education, need a combination of pediatricians and psychologists, psychiatrists to detect and treat the smallest disorders early, limit the risk in the early stages. school section.
In the case of children with low weight and growth retardation, parents should supplement their children with supportive products containing lysine, essential micro-minerals and vitamins such as zinc, chromium, selenium, and B vitamins to help fully meet their needs. nutritional needs in children. At the same time, these essential vitamins also support digestion, enhance nutrient absorption, help improve anorexia, and help children eat well. Parents can simultaneously apply dietary supplements and functional foods derived from nature for easy absorption. The most important thing is that improving your baby's symptoms often takes a long time. Combining many types of functional foods at the same time or changing many types in a short time can make the baby's digestive system unable to adapt and completely not good. Therefore, parents must be really patient with their children and regularly visit the website vimec.com to update useful baby care information.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.