This is an automatically translated article.
The article is expertly consulted by Master, Resident Doctor Dang Thi Ngoan - Pediatrician - Neonatologist - Department of Pediatrics - Neonatology - Vinmec Ha Long International Hospital.When bilirubin rises above the normal range in the blood, the newborn will have a yellow tint to the skin and conjunctiva of the eyes. Cholestatic jaundice is a direct increase in bilirubin due to obstruction of the intrahepatic or extrahepatic bile ducts.
1. Definition of obstructive jaundice in children
Neonatal jaundice due to direct hyperbilirubinemia is defined when:Direct bilirubin concentration > 1mg/dl if TSB<5mg/dl; Direct bilirubin >20% of TSB concentration if TSB >5mg/dl. The cause of neonatal jaundice due to direct hyperbilirubinemia is the liver's inability to excrete bile and/or obstruction of the biliary tree. This condition is also known as cholestatic/obstructive jaundice.
2. Causes of cholestatic jaundice
2.1. Hepatocellular causes Spontaneous neonatal hepatitis Infectious hepatitis: Hepatitis B, a group of infections transmitted from mother to fetus TORCH, congenital syphilis, listeria infection, tuberculosis, .. Toxic hepatitis: Sepsis, intestinal obstruction, prolonged parenteral nutrition, or infarction necrosis; Metabolic pathology: α1-Antitrypsin deficiency, Galactosemia, Tyrosinemia, Fructosemia, Glycogen storage disorder, lipid metabolism disease, Zellweger syndrome, trisomy 21 (excess 1 chromosome 21), trisomy 18 (Edward's syndrome), stasis Advanced intrahepatic bile duct Byler function, primary hypopituitarism,... Hematologic pathology: Placental edema, hereditary blood disorder Congenital Porphyria,... 2.2. Causes of biliary obstruction Extrahepatic biliary atrophy (independent or Trisomy 18); Atrophy of intrahepatic biliary tract; Alagille syndrome; Intrahepatic biliary atrophy with lymphatic edema; Common bile duct cyst...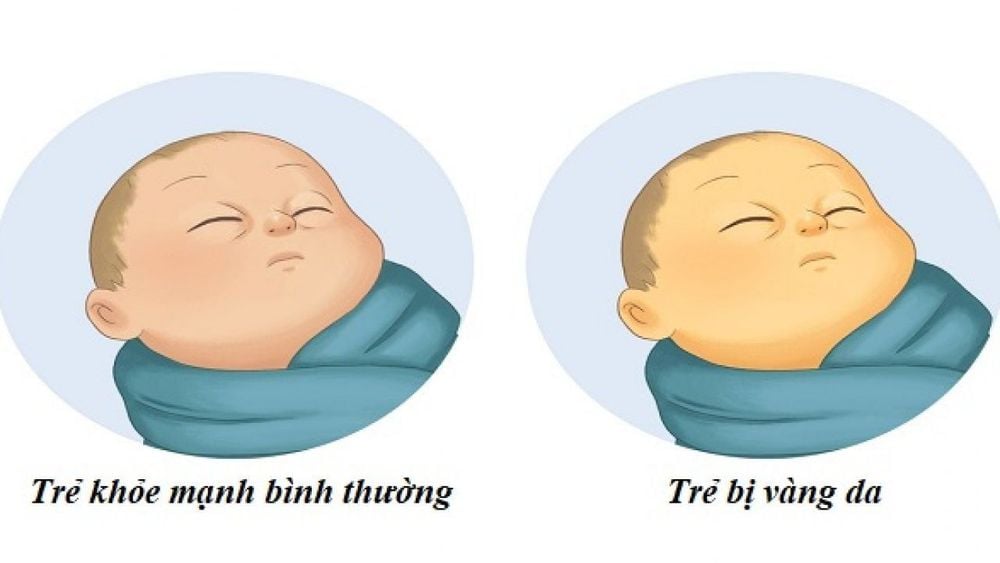
3. Diagnosis of jaundice due to direct hyperbilirubinemia
3.1. History It should be noted whether the child has the following characteristics or not:Fetal infection; Prenatal ultrasound detects abnormalities of the hepatobiliary system and intestinal tract; Immune hemolysis; Neonatal infection (urinary tract, blood or virus); Have ever been breastfed or formula with galactose; Slow weight gain, vomiting, or constipation ; Persistent discolored or clay-like stools (typical of cholestatic jaundice); Dark urine; Hemorrhage; The child's brother/sister has a similar medical condition. 3.2. Clinical examination The following aspects should be fully examined:
Vital signs include pulse, temperature, blood pressure, breathing rate; Development parameters; General condition for malformations of the nose, face and eyes (especially Alagille syndrome); Jaundice; Muscle tone; Fundus examination in children with fetal infection or metabolic disease; Heart murmur (common in Alagille syndrome); Abdominal examination to determine size and density of hepatosplenomegaly, tumor, collateral circulation, umbilical protrusion... Look for signs of hemorrhage; Check the patient's stool and urine. 3.3. Laboratory tests of liver function: total / direct / indirect bilirubin, cholesterol, blood albumin, total protein, protein electrophoresis... Blood tests: complete blood count, peripheral blood smear, pink reticulocytosis, platelets, and whole coagulation; Tests for infection screening: Serological diagnosis of TORCH, hepatitis B in both mother and child, other infection tests depending on the clinical situation; Urinalysis: Urine culture, bile acids in the urine, or abnormal amino acids; Imaging tests: Abdominal ultrasound, hepatobiliary scintigraphy, magnetic resonance cholangiography (MRCP) and endoscopic retrograde cholangiography (ERCP); Supportive tests: Liver biopsy (in children whose diagnosis cannot be confirmed by other tests), duodenal aspiration helps detect biliary obstruction; Other tests: Thyroid function, arterial blood gases, AFP (Alpha-fetoprotein).

4. Treatment of obstructive jaundice in infants
4.1. Principles Specific treatment according to each cause; Supportive/supportive treatment. 4.2. Cause-specific treatment Extrahepatic biliary obstruction: Surgical consultation for Kasai surgery - removal of the damaged extrahepatic biliary tract and replacement with a segment of the child's own small intestine, which acts as a conduit new password. Septic hepatitis: Treatment of infection; Galactosemia (excess galactose in the blood): Adhere to a galactose-free diet. 4.3. Supportive/supportive treatment Provide 125% of the ideal energy by IV or feeding; If oral energy supply: Lipids as medium chain triglycerides; Protein intake: 2-3g/kg/day for children without hyperammonemia; Vitamins: Vitamin A, vitamin D, vitamin E and vitamin K with the dose prescribed by the doctor based on the weight of the child; Ursodeoxycholic acid: 10 - 20mg/kg/day to stimulate bile flow, push and discharge toxic bile acids from the liver.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














