This is an automatically translated article.
The article is written by Specialist Doctor II Nguyen Xuan Thang - Deputy Department of Examination & Internal Medicine cum Head of Inpatient Unit - Vinmec Central Park International General Hospital.
Hyperthyroidism in pregnancy is usually caused by Graves' disease and occurs in 1 - 4 out of every 1,000 pregnancies in the United States. Graves disease is an autoimmune disorder. With this condition, your immune system produces antibodies that cause the thyroid gland to make more hormones than usual.
1. Thyroid physiology during pregnancy
Over 99% of T4 and T3 in the blood are bound to membrane proteins. Only free-form hormones have physiological and metabolic activities. The free hormones make up only a very small amount of the total hormones in the blood, about 0.03% T4 and 0.3% T3.
During pregnancy, the mother's thyroid gland is affected by 3 main factors:
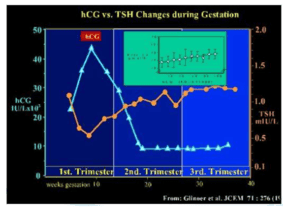
Increased levels of TBG (Thyroid binding globulin): TBG is a transporter of thyroid hormone. Elevated estrogen during pregnancy stimulates the liver to synthesize stem cells. The highest concentration of TBG is at week 21 of pregnancy, 2.5 times higher than normal. Increases hCG levels: hCG consists of two alpha and beta subunits. The alpha subunit is structurally similar to TSH, LH, and FSH. Beta hCG stimulates the TSH receptor as weakly as 1/10000 of that of TSH. hCG peaks around the 10th week of pregnancy (3 - 100 U/L), then gradually decreases until the 20th week of pregnancy (3 - 5 U/L) and stabilizes until childbirth. Multiple pregnancies will lead to an increase in hCG and a decrease in TSH. Peripheral metabolism of thyroid hormone: During pregnancy, thyroid hormone will be de-iodized more than usual due to the action of deidodenase enzyme (types I, II, III), which is abundantly present in the placenta and can The maximum amount is around week 20. Increase in iodine needs and metabolism during pregnancy: Thyroid volume increases by 10% in areas of iodine deficiency, by 20 - 40% in areas of iodine deficiency. Thyroid hormones (T3 and T4) will increase, Iodine requirements will increase by 50% due to an increase in body metabolism, and renal Iodine clearance will also increase by 50% because the fetus also begins to increase Iodine from the mother to synthesize internal organs. thyroid secretions.
2. Causes of pregnancy hyperthyroidism
Hyperthyroidism in pregnant women can be caused by 3 groups:
Basedow's disease: accounted for about 0.1 - 1% (may be present before pregnancy or start in pregnancy). Gestational thyrotoxicosis: accounted for 1 - 3%, there is transient hyperthyroidism in the first half of pregnancy, related to pregnancy status and proportional to hCG concentration (multiple pregnancy, ovum). Other causes include toxic nodular goiter, subacute thyroiditis, troblastoma, and iodine-induced hyperthyroidism.

3. Thyroid function test during pregnancy
FT4 and TSH are accurate diagnostic and monitoring means for thyroid dysfunction in pregnancy.
The value of TSH in pregnancy should have a local reference value. Usually lower than normal during the first 3 months of pregnancy, which varies by ethnicity and testing method. It is recommended that a reference interval be determined for each trimester and by local testing:
Pregnancy TSH Reference Range:
Upper threshold: 2.5 - 3 mIU/L. Lower threshold: 0.1 - 0.2 mIU/L. If no reference value is available, use:
1st trimester: 0.1 - 2.5 mIU/L. Second trimester: 0.2 - 3 mIU/L. Last 3 months of pregnancy: 0.3 - 3 mIU/L.
4. Treatment
Synthetic antithyroid MMI or PTU: Mild cases of hyperthyroidism (when thyroid hormone levels are slightly elevated, symptoms are few) are usually closely monitored without treatment as long as both mother and baby are strong. Both synthetic antithyroid drugs cross the placenta and can impair the baby's thyroid function and cause fetal goiter. Use of synthetic antithyroid drugs during the first trimester of pregnancy is associated with birth defects, although PTU-related malformations are less frequent and less severe. It is recommended that the lowest possible dose of synthetic antithyroid drugs be used to control maternal hyperthyroidism in order to minimize the development of hypothyroidism in the infant. Overall, the benefits to the baby from treating a mother with hyperthyroidism during pregnancy outweigh the risks if the therapy is carefully monitored.First 3 months of pregnancy should be used PTU (preferred to 16 weeks) 2nd trimester can continue PTU or switch to MMI. 3rd trimester: MMI is more commonly used because of the risk of liver fibrosis when using PTU in both mother and baby. Surgery: In patients who require treatment but cannot be adequately treated with antithyroid drugs, surgery is an acceptable alternative. Thyroidectomy is safest in the second trimester of pregnancy (between 4 and 6 months).
Radioactive iodine: Contraindicated to treat hyperthyroidism during pregnancy because it can cross the placenta and cause gland destruction and lead to permanent hypothyroidism.
Beta-blockers: May be used minimally appropriately during pregnancy to help treat palpitations and tremors caused by hyperthyroidism. Usually, these drugs are prescribed only until the hyperthyroidism is controlled with antithyroid drugs.

5. Risks of hyperthyroidism to mother and fetus
Hyperthyroidism can start in the first trimester or get worse during this period in women with pre-existing conditions. Untreated maternal hyperthyroidism can cause premature labor, serious complications that are preeclampsia, thyroid storm. Uncontrolled maternal hyperthyroidism is associated with fetal tachycardia, small for gestational age, preterm birth, stillbirth, and birth defects. In addition, very high levels of thyroid-stimulating immunoglobulin (TSI) can affect the fetus. Basedow's disease is an autoimmune disease caused by the production of thyroid-stimulating antibodies (TSI). These antibodies cross the placenta and may interact with the fetal thyroid gland. High levels of TSI in maternal blood can cause fetal hyperthyroidism or neonatal hyperthyroidism, but are uncommon. However, this condition only occurs when the mother's TSI concentration is many times higher than normal. Measurement of the TSI level in the blood of mothers with Graves' disease is recommended early in pregnancy and, if elevated at first, repeat a second time around 18-22 weeks of gestation.6. Monitoring pregnancy
Ultrasound of fetal thyroid. For signs of hypothyroidism after 20 weeks, the lowest possible antithyroid dose should be used with the goal of maintaining maternal blood FT4 within the upper limit of normal because all antithyroid drugs cross the placenta and affect the fetus. pediatric. Thyroid function tests (TSH and thyroid hormone levels) monthly. Basedow may improve in the third trimester of pregnancy and may worsen postpartum. Maternal TRAb measurement during the last 3 months of pregnancy (24 to 28 weeks) predicts fetuses at high risk of developing neonatal and fetal hyperthyroidism. If pregnant women have symptoms such as unexplained rapid weight loss, sweating, rapid heart rate, fatigue, eye irritation, frequent bowel movements or diarrhea, ... or symptoms related to stress. thyroid, it is best to go to a large hospital to be diagnosed and tested to evaluate thyroid function.
Currently, Vinmec International General Hospital is the address where customers can go to perform tests to evaluate thyroid function and treat diseases actively and effectively. The hospital's Endocrinology Department is a gathering place of experienced doctors, solid expertise and always devoted to the patient's health. At the same time, the hospital is also equipped with a system of modern medical equipment, comfortable facilities, the best support for the diagnosis and treatment of diseases.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














