This is an automatically translated article.
Cervical cancer is the 4th most common cancer for women worldwide, but over time it has become one of the most preventable cancers. So when and how should cervical cancer screening be done?1. What is cervical cancer?
Cervical cancer is cancer that starts in the cervix - the narrow opening connecting the vagina and uterus. The normal intracervical neck will be a healthy pink color with a thin, flat layer of squamous cells. The cervical canal is made up of another type of cell called a columnar cell. The area where these two types of cells meet is called the transition zone, which is where abnormal or precancerous cells are most likely to develop.
Most cervical cancers (80 - 90%) are squamous cell carcinomas. Adenocarcinoma is the second most common form of cervical cancer, accounting for 10-20% of cases. This form of cancer develops from the mucus-secreting glands in the cervical canal. Although less common than squamous cell carcinoma, the incidence of adenocarcinoma is increasing, especially in younger females.
Each year more than 13,000 women in the United States are diagnosed with cervical cancer, and more than 4,000 die. Cervical cancer deaths in the United States continue to decline by about 2% per year. This decline is mainly due to the widespread adoption of the Pap test (ThinPrep Pap or Pap smear) to detect cervical abnormalities and enable early treatment. Most women with abnormal cervical cell changes that progress to cervical cancer have never had a Pap test or haven't had a test in the three to five years before their cancer diagnosis.
Cervical cancer tends to occur in middle age. It is usually diagnosed in women between the ages of 35 and 44. The disease rarely affects women under 20 years of age, and more than 15% of diagnoses are made in women over 65. But in the group of women over 65, the cancer was more common in women who didn't have regular screening tests.
Trắc nghiệm: Bạn biết gì về các yếu tố nguy cơ, chẩn đoán và điều trị ung thư tuyến tụy?
Ung thư tuyến tụy phổ biến thứ 10 trong những bệnh ung thư mới và là nguyên nhân thứ 4 gây tử vong do ung thư ở nam, nữ. Bài trắc nghiệm này sẽ kiểm tra kiến thức của bạn về các yếu tố nguy cơ, chẩn đoán và cách điều trị ung thư tuyến tụy.
Bài viết tham khảo nguồn: medicalnewstoday 2019
2. Cervical cancer screening
2.1. Causes of cervical cancer
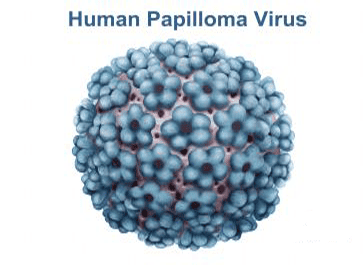
Most cases of cervical cancer are caused by infection with the HPV virus. HPV is a virus that enters cells and can cause cells to mutate. Certain types of HPV have been linked to cervical cancer as well as cancers of the vulva, vagina, penis, anus, mouth, and throat. The strains of HPV that can cause cancer are called "high-risk strains."
HPV is transmitted from person to person during sexual activity. This is very common and most people who have sex will get HPV in their lifetime. HPV infection usually causes no symptoms. Most HPV infections go away on their own. These short-term viral infections usually cause only mild (low-grade) changes in cervical cells. The cells return to normal when the HPV infection is cleared up. But in some women, HPV doesn't go away. In cases where a person is infected with a high-risk strain of HPV that persists for a long time, it can cause more severe (high-risk) changes in cervical cells. These changes are more likely to lead to cancer.
2.2. Why is cervical cancer screening so important?
It usually takes 3-7 years for high-risk changes in cervical cells to turn into cancer. Cervical cancer screening can detect these changes before they become cancerous. Women with low-risk changes may be tested more often to see if their cells return to normal. Women with high-risk changes may be treated to remove the cells.
2.3. So how is cervical cancer screening done?
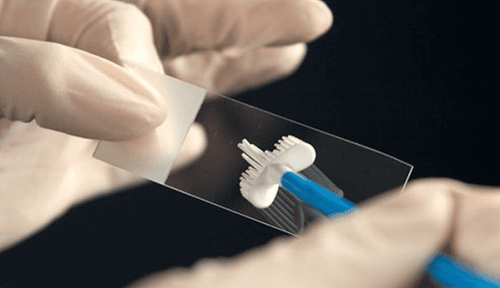
Cervical cancer screening includes a Pap test (ThinPrep Pap or Pap smear, depending on your doctor's orders), and for some women, an HPV test. Both tests use cells taken from the cervix. The screening process is simple and fast. You lie on a special chair and a device called a speculum is used to open the vagina. The speculum gives the doctor a clear view of the cervix and upper part of the vagina.
The doctor will use a specialized brush or other device to collect samples for testing. This sample of cervical cells will be stored in a tube containing a special solution and sent to the laboratory.
For the Pap test (ThinPrep Pap or Pap smear), the sample will be checked for the presence of abnormal cells.
For HPV testing, the sample will be tested for the presence of 13-14 high-risk strains of HPV.

2.4. How often should cervical cancer screening and what tests should be done?
When and what type of test depends on your age and medical history.
Females aged 21 - 29 should have a Pap test (ThinPrep Pap or Pap smear) every 3 years. HPV testing is not recommended.
Women aged 30 - 65 years should have a Pap test and HPV test at the same time every 5 years (preferred). Or you can have a Pap test every 3 years.
2.5. When should cervical cancer screening be stopped?
Women should stop cervical cancer screening after age 65 if there is no history of moderate or high abnormal cervical cells or malignancy and you have had three negative Pap test results consecutive or two consecutive co-negative test results within the last 10 years, and the most recent result taken within the last 5 years.
2.6. If I have had a hysterectomy, do I need to be screened for cervical cancer?
If you have had a hysterectomy, you may still need screening. This decision is based on whether the cervix has been removed, the reason for the need for hysterectomy, and whether there is a history of moderate or severe cervical cell changes or cervical cancer.
Even if the cervix has been removed at the time of hysterectomy, cervical cells may still be present at the top of the vagina. If there is a history of cervical cancer or cervical cell changes, screening should continue for the next 20 years from the time of surgery.
2.7. Are there any circumstances under which these routine cervical cancer screening guidelines should not be followed?
Women with a history of cervical cancer, human immunodeficiency virus (HIV) infection, weakened immune systems, or prenatal exposure to diethylstilbestrol (DES) may need more frequent screening and these routine instructions should not be followed.
This screening recommendation also applies to patients who have been vaccinated against HPV. Women who have been vaccinated against HPV still need to follow age-group screening recommendations.
2.8. What to do if there are abnormal cervical cancer screening test results?
Many women have abnormal cervical cancer screening results. An abnormal result does not mean cancer. Cervical cell changes usually return to normal. And if they don't return to normal, it usually takes several years for the high-risk changes to become cancerous.
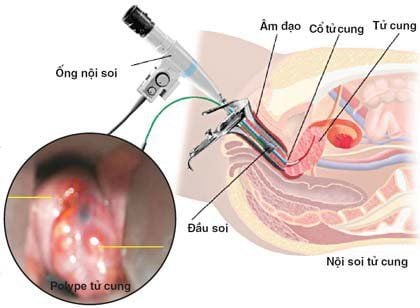
If there are abnormal screening test results, additional testing needs to be ordered to find out if high-risk changes or cancer are indeed present. Sometimes, just repeating the test is enough. In other cases, colposcopy and cervical biopsy may be recommended to find out the severity of these changes.
If follow-up test results show high-risk changes, you may need treatment to remove the abnormal cells. Follow-up testing is needed after treatment and will need to be checked for cervical cancer regularly once the follow-up is complete.
2.9. How accurate are cervical cancer screening test results?
As with any other lab test, cervical cancer screening results are not always accurate. Sometimes, the results show abnormal cells while the cells are normal. This is called a “false positive” result. Cervical cancer screening may also fail to detect abnormal cells when they are present. This is called a “false negative” result.
To help prevent false-negative or false-positive results, patients should avoid douching, sex, and using vaginal suppositories or hygiene products for 2 days before the test. Also avoid having cervical cancer screening tests while you are menstruating.
References source: American Association of Obstetricians and Gynecologists
Acog.org
See also:
Can cervical cancer be cured? Early stage cervical cancer can be cured immediately if detected early Cervical cancer treatment in stages