This is an automatically translated article.
Endometrial polyps are quite common disease in women. Most of the diseases are benign and do not cause any discomfort to the patient. However, in some cases, the disease can cause uterine bleeding or adversely affect menstrual status, even affecting a woman's fertility and pregnancy.
1. What are endometrial polyps?
Endometrial polyps usually appear in women of reproductive age or perimenopause. Most women with endometrial polyps are benign. Polyps are small, rather soft growths that develop in the endometrium. Polyp formation is caused by an overgrowth of the inner lining of the uterus or the endometrium. Usually, endometrial polyps have a stalk that connects to the wall of the uterus, with a blood vessel in the middle of the stalk to supply blood to the polyp. Polyps can develop in any part of the uterus.
The size of endometrial polyps can range from a few millimeters to several centimeters, or there can be one or more polyps.
Endometrial polyps often have signs of abnormal bleeding, or dull abdominal pain in the lower abdomen or anemia if bleeding is prolonged and repeated. The cases of patients with endometrial polyps are usually detected during routine health check-ups with uterine biopsy or CTC cytology.
Polyps and fibroids have many similarities, but there are also a few differences. Fibroids are an overgrowth of muscle inside the uterine wall, not the inner layer of tissue. Like polyps, they can cause heavy bleeding. However, they can also cause pain, constipation, and difficulty urinating. The same tests can find fibroids and polyps. Your doctor will be able to see what disease you have and recommend the best treatment.
2. What causes endometrial polyps?
Although the causes of polyps are still not clear. But the majority of cases are thought to be related to increased levels and effects of endogenous or exogenous estrogen. Women with a body mass index greater than 30 were overweight and obese and also had a 55% incidence of endometrial polyps. The use of breast cancer drugs such as Tamoxifen also increases the risk of endometrial polyps. Other factors may increase the risk of endometrial polyps, such as hormone replacement therapy in women. women who have gone through menopause that contain estrogen, or Lynch and cowden syndrome....
Endometrial polyps may not be immediately dangerous to the patient, but if not treated promptly. and can definitely cause complications affecting a woman's reproductive health. The dangers that may occur with cases of endometrial polyps such as infertility in women due to the obstruction of the implantation of the fertilized egg in the uterus, causing chronic anemia due to uterine bleeding or can affect a woman's pregnancy because endometrial polyps grow large, creating pressure on the fetus and can even lead to miscarriage or premature birth.
In addition, this condition can cause inflammation-related diseases such as vaginitis, vulvovaginitis, cervicitis, etc., all of which are caused by the process of increasing secretions. Worse cases, with a very small number of polyps can progress to cancer.
3. Symptoms of endometrial polyps
Endometrial polyps often have the following signs or symptoms:
Abnormal uterine bleeding (AUB) in about 64 to 88% of cases with endometrial polyps have AUB. This bleeding is characterized by mid-cycle, or it can be heavy bleeding during the period - hypermenorrhoea. Uterine bleeding accompanied by abdominal pain and anemia. Some cases may not have obvious symptoms, but are often discovered incidentally during infertility investigation or through cervical cytology tests, or performing uterine biopsy.
4. Diagnosis of endometrial polyps
One of the most commonly used diagnostic methods for uterine polyps is abnormal bleeding or a woman with a history of infertility or miscarriage.
With symptoms that may suggest that the doctor suspects endometrial polyps, the doctor will order one or more tests to differentiate it from other causes such as:
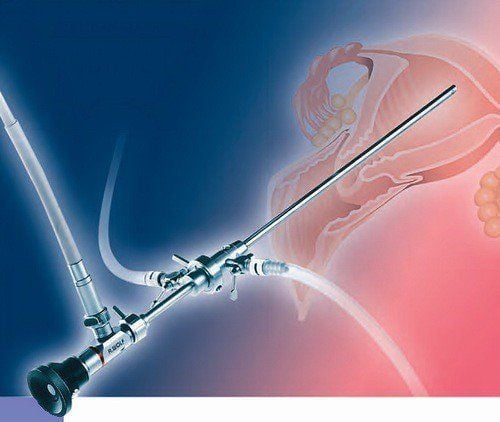
Transvaginal ultrasound Vaginal intubation to obtain images in this position. The doctor will see a polyp with a very prominent stalk or may be suspicious when the endometrial layer is thicker than normal. Ultrasound injects water into the ovary with the use of saline to inject into the lumen of the uterus, while at the same time dispensing the uterine cavity. Next, ultrasound will be used to reconstruct the image and observe the abnormal structures in the uterine cavity as well as in the position of the wall of the uterus. During an endometrial biopsy, your doctor may take one or more tissue samples from this area to find the cause of an infection or cancer of the uterus. Hysteroscopy involves the doctor doing this procedure with a small endoscope inserted through the vagina and cervix and then into the ovaries. In addition, the doctor can use a number of instruments along with the endoscope that can be inserted and cut and removed during the colonoscopy. Apply the curettage. The doctor will use a metal instrument with a small ring on the end to take a small sample of polyps or tissue in the uterus for testing, and use the curettage to remove the polyp.
6. Methods to treat endometrial polyps
For women with endometrial polyps smaller than 10mm and no clinical symptoms, about 6.3% of women with polyps can regress on their own. Therefore, to treat endometrial polyps, there are currently 2 methods including medical treatment method and surgical treatment method.
6.1. Medical treatment Medical treatment will be using an IUD containing Levonorgestrel ingredient that can prevent the formation of endometrial polyps, especially in cases where tamoxifen is used. Or, systemic progesterone can be used in the medical treatment of endometrial polyps, when GnRH agonists act on the endometrium. However, this case is only to use pre-intervention supportive treatment with surgical treatment.
6.2. Surgical treatment of endometrial polyps is done through the following cases:
Occurrence of symptoms and polyp size larger than 1.5cm The progressing condition is multiple polyps Polyps protruding from the cervix Polyps in case Infertility, miscarriage, and curettage can also help remove polyps. However, this method is considered a "blind" procedure because the exact location of the polyp cannot be seen. This also means that it is not certain to completely remove the polyp. In addition, it is possible that crumbling tissue causes difficulties in histological evaluation.
Endometrial polyps can be treated with 76-100% improvement in symptoms and low recurrence. Besides, this condition can also improve a woman's chances of getting pregnant by 43 to 80%. However, in postmenopausal women, endometrial polyps may pose a greater risk of malignancy. Therefore, in these subjects, when detecting endometrial polyps with or without symptoms, polypectomy should be indicated immediately.
Vinmec International General Hospital is the address for examination, treatment and prevention of diseases, including Obstetrics and Gynecology. When performing the examination process at Vinmec, customers will be welcomed and used modern facilities and equipment along with perfect medical services under the guidance and advice of experts. Good doctors, well-trained both at home and abroad. Therefore, when you have symptoms of endometrial polyps or other abnormalities, you can go to Vinmec for a thorough examination and treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: webmd.com