This is an automatically translated article.
The article was professionally consulted by Doctor Tran Thi Diem Trang - Respiratory Internal Medicine Doctor - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital. The doctor has more than 10 years of experience in the treatment of respiratory diseases.Emphysema and chronic obstructive pulmonary disease are closely related. All people with emphysema have chronic obstructive pulmonary disease, but chronic obstructive pulmonary disease can include many other conditions that are unlikely to be caused by emphysema.
1. What is emphysema?
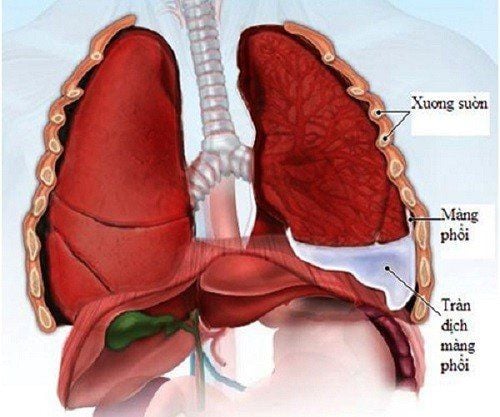
Emphysema is a form of chronic obstructive pulmonary disease. Emphysema causes difficulty breathing because the lung sacs are damaged for a long time, causing the alveoli to weaken and burst, replacing a small space with a large space, reducing the surface area of the lung, reducing the amount of oxygen entering the blood. When the patient exhales, the damaged alveoli cannot function properly, making oxygen-rich air outside the lungs unable to enter the lungs, on the contrary, the air inside the body cannot be pushed out, creating lack of oxygen in the blood, difficulty breathing.The main cause of emphysema is smoking and smoking. Besides, there are a number of causes such as exposure to the environment with lots of dust, toxic chemicals...
2. What is Chronic Obstructive Pulmonary Disease (COPD)?
Chronic obstructive pulmonary disease is a condition in which the airways narrow, making it difficult to breathe. Chronic obstructive pulmonary disease (COPD) is a progressive disease, which means it gets worse and can even be life-threatening.Chronic obstructive pulmonary disease is divided into two types, including:
Chronic bronchitis: A condition in which the lining of the bronchial tubes becomes inflamed. The lining in the bronchopulmonary tubes is swollen, red, and filled with mucus. This mucus is the cause of the narrowing of the airways Emphysema: emphysema damages the air sacs (alveoli) in the lungs and gradually destroys them, making it harder for the person to breathe. When the alveoli in the lungs are destroyed, the process of exhaling CO2 and absorbing O2 will become more difficult because the outside air entering the body is obstructed, and the air in the body is not able to escape smoothly. . As a result, the patient finds it difficult to breathe. Chronic obstructive pulmonary disease is very dangerous. The lungs have two main organs, the bronchi and the alveoli, also known as the airways and the air sacs, respectively. In addition, there is a trachea. When you inhale, air moves from the trachea to the alveoli through the bronchial tubes. From there, oxygen enters the blood and CO2 is pushed out through the alveoli. If there is any problem that interrupts the above gas exchange, the patient will have difficulty breathing.

3. Relationship between emphysema and chronic obstructive pulmonary disease
Emphysema and chronic obstructive pulmonary disease are closely related. People with emphysema can develop chronic obstructive pulmonary disease. Emphysema is a form of chronic obstructive pulmonary disease.Most people with emphysema also have chronic bronchitis. Chronic bronchitis will cause the patient to have a persistent cough. Chronic bronchitis and emphysema are two conditions that lead to chronic obstructive pulmonary disease.
Smoking is the leading cause of emphysema and chronic obstructive pulmonary disease. The damage of emphysema and chronic obstructive pulmonary disease are both irreversible damage that can only slow the progression of the disease.
4. Distinguishing symptoms of emphysema and chronic obstructive pulmonary disease
Signs of emphysema include:Persistent, unrelenting cough Shortness of breath Shortness of breath. Chest tightness Fatiated barrel-shaped chest. Pale skin, blue fingers and nails Decreased immune system increases risk Pneumonia The first symptom of COPD patients is a persistent cough with phlegm in the morning. Patients often do not pay attention and think that this is a normal symptom because smoking causes patients to subjectively not go to the doctor. However, some patients with COPD have no persistent cough and expectoration.
The next symptom will be shortness of breath on exertion. Dyspnea on exertion first appears when the patient goes up stairs, when walking quickly on level roads, then slower than people of the same age. Patients with COPD often change unconsciously to avoid doing activities and tasks that make it difficult for them to breathe. Even if a patient develops shortness of breath on exertion, they may not see a doctor because they think this is normal due to old age. And when the patient comes to the doctor, usually the respiratory function has decreased a lot.
The next symptom will be the times of COPD exacerbation, the patient has more difficulty breathing, more sputum, cloudy color. These exacerbations are getting more and more frequent, closer together, longer duration.
Systemic symptoms gradually appear as COPD worsens.
Thinness, weight loss, exhaustion mainly Skeletal muscle atrophy Osteoporosis due to systemic inflammatory process, due to prolonged use of corticosteroids. Depression. Isochromic, isochromic microcytic anemia Increases the risk of cardiovascular diseases such as myocardial ischemia, myocardial infarction. Clinical symptoms of COPD are varied and develop silently, patients often go to the doctor when the disease is severe.

5. Diagnosis of emphysema and chronic obstructive pulmonary disease
5.1. Diagnosing emphysema When going to the doctor to diagnose emphysema, the doctor will ask about the patient's symptoms and medical history. In addition, the patient needs to let the doctor know if he or she smokes, works or lives in a polluted environment. This is one of the risk factors for emphysema.Tests to diagnose emphysema include:
Computed tomography CT Chest X-ray Pulmonary function test Arterial blood gas test Electrocardiogram to determine if there is a heart problem 5.2. Diagnosis of Chronic Obstructive Pulmonary Disease The diagnosis of chronic obstructive pulmonary disease is based on symptoms, medical history, and family history. In addition, doctors will conduct clinical examination and assign patients to perform tests.
The doctor will use a stethoscope to check the lungs for wheezing or other unusual sounds in the lungs.
Diagnostic tests for chronic obstructive pulmonary disease include:
Pulmonary function test : Measures the amount of air the patient inhales and exhales, to check if the patient has difficulty breathing, the lungs are fully supplied enough oxygen for the body's activities not Measure the spirometer : Check breathing ability, use the device to measure the amount of exhaled air, breathing rate CT scan, chest X-ray : Observe the images of the lateral structures in the chest to detect signs of chronic obstructive pulmonary disease Arterial blood gases : Blood tests, which measure the level of oxygen in the blood
6. Treatment of emphysema and chronic obstructive pulmonary disease

Stop smoking Using drugs such as drugs: bronchodilators, steroids, antibiotics... Therapies: pulmonary rehabilitation, nutritional therapy or supplemental oxygen to improve breathing Lung volume reduction surgery Flu and pneumococcal vaccinations are available 6.2. Treatments for Chronic Obstructive Pulmonary Disease Like emphysema, there is no cure for chronic obstructive pulmonary disease. Treatment goals for chronic obstructive pulmonary disease:
Slow the progression of COPD. Alleviate symptoms. Increase exercise capacity. Enhance general health status. Prevention and treatment of complications of COPD. Prevention and treatment of COPD exacerbations. Reduce mortality. Specifically,
Non-pharmacological treatment:
CANCELING: > 1/3 of COPD patients continued to smoke when the disease was detected. Smoking cessation slows the progression of COPD at any stage of the disease and reduces the annual rate of decline in FEV1. Flu shot: The flu can be a problem in patients with COPD. When a patient has a cold, COPD may worsen during exacerbations. The flu shot reduces the risk of catching a cold, given it once a year between September and October. REVOLUTIONARY RECOVERY: COPD patients should attend a training course on how to practice physical therapy to practice breathing and expectoration. Pinch breathing and diaphragmatic breathing are very beneficial for the patient. Drug treatment: the basic drugs used are bronchodilators:
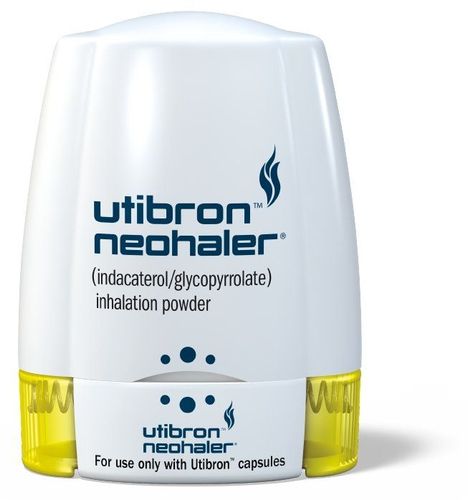
Short-acting bronchodilators indicated for COPD stage A or higher when the patient has symptoms of cough, shortness of breath: Salbutamol group = VENTOLIN®. Anticholinergic group: Ipratropium Bromide = ATROVENT®. Anticholinergic and Salbutamol combination group in the same inhaler: Ipratropium Bromide + Fenoterol = BERODUAL®; Ipratropium Bromide + Salbutmol = COMBIVENT®. Long-acting bronchodilators are indicated for COPD stage B or higher, used regularly throughout the day regardless of symptoms of cough, shortness of breath or not. Tiotropium Bromide = SPIRIVA®. Tiotropium + Olodaterol = SPIOLTO A long-term bronchodilator can also be replaced by a short-acting bronchodilator at regular intervals.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.