This is an automatically translated article.
The article was professionally consulted by a Doctor of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalParkinson's disease is a degenerative disease of the nervous system that affects the body's ability to move. Symptoms begin slowly, often starting with tremors in just one hand, which can initially be very mild and unnoticed by the patient. Parkinson's disease symptoms will get worse as the disease progresses over time. Although Parkinson's disease cannot be cured, medication can significantly improve symptoms.
1. Diagnosis of Parkinson's disease
There is no specific test to accurately diagnose Parkinson's disease. To diagnose Parkinson's disease, doctors must be trained in neurology. Diagnosis of Parkinson's disease is based on medical history, review of current signs and symptoms, neurological and general examination. The clinical examination procedures help the doctor to guide the diagnosis of Parkinson's disease, and it is the symptoms and signs obtained from the neurological examination that will largely support the doctor's diagnosis and identification of the disease.
In addition, the Doctor may order investigations such as blood tests or MRI, CT and PET imaging techniques to rule out other conditions that can cause symptoms similar to Parkinson's disease. .
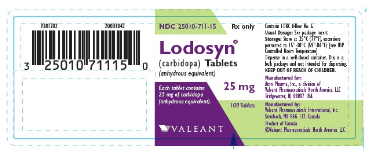
In addition to the physical examination, to diagnose Parkinson's disease, the doctor may test the response to carbidopa-levodopa by giving the patient carbidopa-levodopa (Rytary, Sinemet or others) and then assessing the response to the drug ( Levodopa test). Patients will be given doses just enough to show whether taking the drug improves symptoms of Parkinson's disease. If symptoms improve significantly with the drug carbidopa-levodopa, Parkinson's disease can be diagnosed.
Sometimes it takes a while for a patient to confirm Parkinson's disease, so a neurologist may recommend follow-up visits to regularly assess progress of the disease over time in order to promptly diagnose correctly and treat Parkinson's disease according to the following regimen.

Chụp PET trong chẩn đoán bệnh Parkinson
2. How to cure Parkinson's disease?
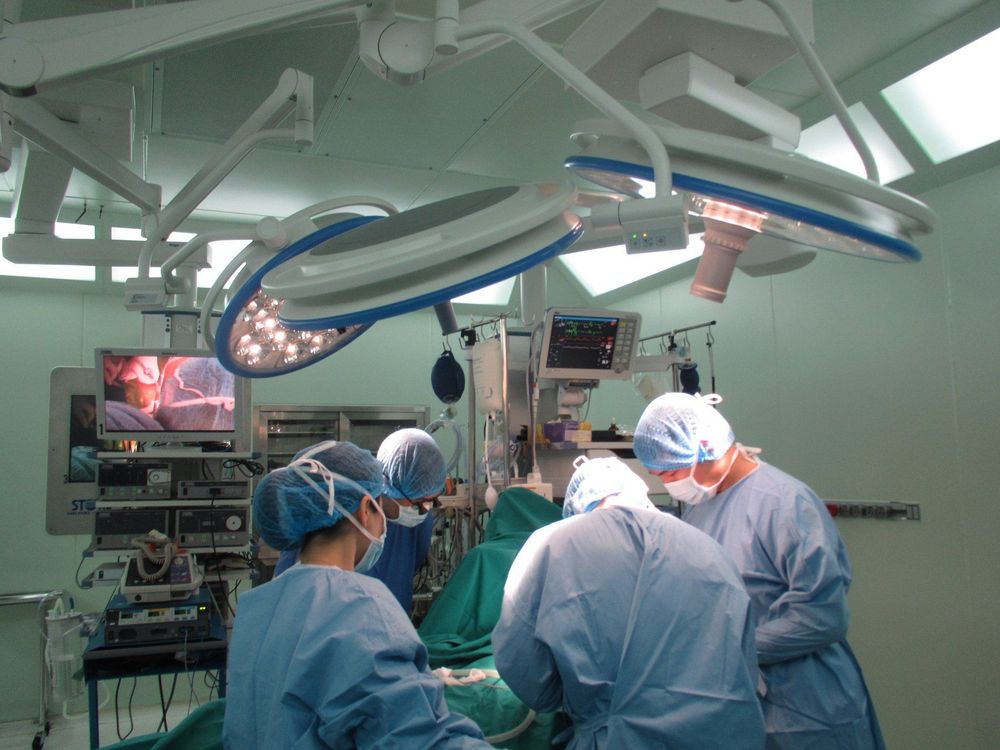
Parkinson's disease cannot be cured, but medication can significantly help control symptoms. For more severe cases, surgery (deep brain stimulation,...).
The doctor may also recommend lifestyle changes, especially regular exercise. In some cases, performing physical therapy that focuses on balance and stretching is also important. In addition, the person may also need the assistance of a speech therapist to help with speech problems.
2.1 Medication Medicines can help people with symptoms that cause gait, mobility, and tremor problems. These drugs increase the concentration or substitute for dopamine in the brain because people with Parkinson's disease have low endogenous brain dopamine sources.
After using the drug, the symptoms will improve significantly, however, over time, the effect of these drugs often fades or the patient responds poorly to the drug. Doctors usually prescribe the following drugs:
Carbidopa-levodopa. Levodopa is the most effective drug for Parkinson's disease, this is an active substance that after entering the patient's brain will be converted into dopamine. Side effects may include nausea or dizziness (orthostatic hypotension). Dopamine agonists (dopamine agonists). Unlike levodopa, dopamine agonists do not convert to dopamine, instead, they mimic the effects of dopamine in the brain. Although not as effective as levodopa in treating symptoms, dopamine agonists last longer and can be used with levodopa to further reinforce the effects of levodopa. Some of the side effects of dopamine agonists are similar to those of carbidopa-levodopa, with other side effects such as hallucinations, drowsiness, hypersexuality, gambling, and addiction. Eating. Monoamine oxidase inhibitors are intended to help prevent the breakdown of dopamine in the brain by inhibiting the enzyme monoamine oxidase B (MAO B). This enzyme is responsible for the metabolism of dopamine in the brain. Side effects may include nausea or insomnia. Catechol O-methyltransferase (COMT) inhibitors. This medication prolongs the effects of levodopa by blocking an enzyme that breaks down dopamine. Anticholinergic drugs. These drugs have been used for many years to help control tremors caused by Parkinson's disease. Several anticholinergic drugs are available, including benztropine (Cogentin) or trihexyphenidyl. Amantadine. Doctors may prescribe amantadine alone to ease the symptoms of Parkinson's disease in the early stages. And is often used with carbidopa-levodopa. 2.2 Deep brain stimulation In deep brain stimulation surgery, surgeons implant electrodes in a specific part of the patient's brain. The electrodes are connected to a generator, which is implanted in the chest near the patient's collarbone. This machine is responsible for sending electrical impulses to the implantation of electrodes in the brain and helps relieve symptoms of Parkinson's disease.
The doctor can adjust the device's settings to suit each patient's condition. However, surgery has some complications such as infection, stroke or brain hemorrhage. Some people have problems with their deep brain stimulation systems or have complications from stimulation that may require a doctor to adjust or replace some parts of the device.
Deep brain stimulation is often indicated for people with advanced Parkinson's disease who have had a poor response to medication (eg, levodopa). The Deep Brain Stimulation System can reduce motor complications of drugs, reduce or halt movement disorders, reduce tremors, decrease stiffness, and improve slow motion.
Although a deep brain stimulation system can provide long-term benefits for Parkinson's symptoms, it cannot stop Parkinson's disease from progressing.
Phẫu thuật kích thích não sâu
3. Caring for Parkinson's patients
Parkinson's disease in the elderly often causes problems with movement in daily activities. But the exercises below are very simple, which can help patients move and walk more safely.
To improve walking
Walk carefully. Don't move fast. Let your heels touch the ground first. Always stand up straight. To avoid falling
Do not go backwards. Do not hold or wear items while walking. Try to avoid leaning over. To turn around, perform a U-shape. Do not rotate your heels. Remove all objects that increase the risk of tripping in the home. When getting dressed
Take extra time to get dressed and don't rush. Choose clothes that are easy to put on and take off. Try using clothes or shoes that have velcro instead of buttons or buttons or shoelaces. Try wearing pants and skirts with elastic bands.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Articles refer to sources: mayoclinic.org, healthline.com, who.int