This is an automatically translated article.
The article was written by Doctor Ngo Van Dan - Department of Neonatology - Vinmec Times City International General Hospital.
Signs of conjunctivitis in children can come as: red, possibly pus-filled, swollen conjunctiva. Children often feel itchy, uncomfortable, children often rub their eyes.
1. Diagnosis of conjunctivitis due to occlusion of the lacrimal gland?
Children with blocked tear conjunctivitis often have some of the following signs:
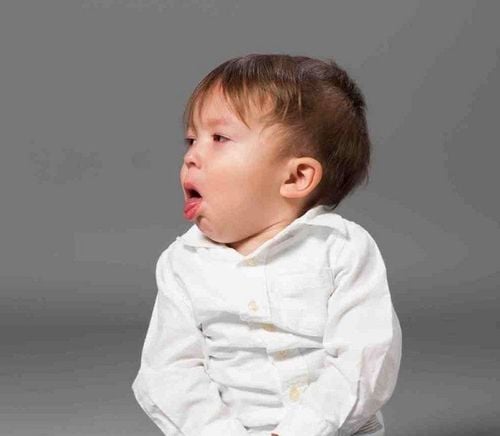
Newborns often have watery and watery eyes. The phenomenon of tears (not crying) will be more when it is cold, windy or sunny... Especially, every morning when children wake up, their eyes often have a lot of yellow rust sticking around the eyelids. Children's eyes are always wet as if they have just cried due to tears in the slits of the eyelids. Signs of conjunctivitis: red, possibly pus-filled, swollen conjunctiva. Children often feel itchy, uncomfortable, children often rub their eyes. Signs of tear duct obstruction are easily recognized or not due to complete or partial obstruction. If partially blocked, it may take a while for the young parents to notice the "special" in their child's eyes.
2. What tests should be done?
The ophthalmologist will take a medical history, do a thorough eye exam, and use a number of methods to assess whether the lacrimal gland is blocked, and what is causing it. The doctor will use a specialized eye examination lamp to check the condition of the child's conjunctiva and cornea. The doctor will inject fluid into the lacrimal system through the tear point in the inner corner of the affected eye. If this amount of fluid does not reach the throat, the child is diagnosed with tear duct obstruction. Other tests, such as X-rays or CT scans with contrast injection into the lacrimal system, may be used when the doctor needs to investigate further.

3. Treatment of conjunctivitis caused by tear duct obstruction
Treatment of conjunctivitis:
Children diagnosed with conjunctivitis will be prescribed eye drops, including topical antibiotics. Families need to pay attention to using prescription drugs, avoid letting children touch their eyes (will make more infections). After a few days of treatment, the condition will improve.
Treatment of lacrimal occlusion:
Many cases of congenital lacrimal occlusion will improve on their own within a few months after birth as the baby's tear drainage system is more complete or when the membrane covering the lacrimal duct opens. In some cases, the ophthalmologist will instruct parents to press down along the side of the child's nose to dislodge the membrane. Most cases of lacrimal occlusion following facial trauma will not require supportive treatment because the tear drainage system usually takes several months to work on its own. As a result, your ophthalmologist will likely recommend waiting several months before considering surgery. In children whose obstruction does not improve on its own, the physician will intervene by conventional methods. An instrument will be used to dilate the lacrimal site before the catheter is inserted through the lacrimal duct. The stick will be threaded down to the nose and then withdrawn. Then, the lacrimal canal will be flushed with physiological saline to flush out the stagnation causing stuffiness. For cases where the canal is blocked due to inflammation or scar tissue, the doctor will use a small tube to thread it into the lacrimal canal down to the lacrimal canal, inflate the balloon so that the balloon at the tip of the tube bulges out to widen the narrow spot. , then discharge the ball. This procedure requires general anesthesia. Another method, which also requires general anesthesia, is called the intubation method. The doctor will insert a small piece of wire into the lacrimal canal through one or both of the tear points in the inner corner of the eye, then thread it completely down the nose and stay like that for 3 to 4 months. The end of the tube at the tear point is knotted to keep the rope from slipping off. This knot will not cause discomfort. Surgery is often the choice of advanced tear duct obstruction. This method is also quite effective for children with congenital tear duct obstruction. However, it is applied after the above methods fail. The use of nasolacrimal bags is used to treat most cases of lacrimal occlusion. The doctor will create a connection point between the tear sac and the nose. As a result, tears will no longer flow down the nasal tear duct, where it is blocked, as before, but directly into the nose through the new passage. In order for the anastomosis to be stable, the doctor will put the tube in and keep the tube for 3 to 4 months before taking it out. Depending on the location of the blockage, the surgeon may create an opening right from the tear point and lead straight into the nose, bypassing the entire lacrimal system below. This method is called lacrimal conjunctival (or lacrimal) conjunctiva. To prevent infection after surgery, the child will need to use nasal vasoconstrictors and eye drops. After 3 to 6 months, the tube placed inside will be removed. If the tear duct obstruction is due to tumor compression, surgical removal of the tumor or other methods to reduce the size of the tumor will be performed to address the cause.

Pediatrics department at Vinmec International General Hospital is the address for receiving and examining diseases that infants and young children are susceptible to: viral fever, bacterial fever, otitis media, pneumonia in children, .... With modern equipment, sterile space, minimizing the impact as well as the risk of disease spread. Along with that is the dedication from the doctors with professional experience with pediatric patients, making the examination no longer a concern of the parents.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.