This is an automatically translated article.
Diabetic retinopathy is a major cause of blindness in developed countries and is becoming increasingly common in developing countries.Diabetic retinopathy occurs in 90% of diabetes cases that develop after 10 to 15 years, regardless of whether or not the diabetes is insulin dependent. Over 200 million people worldwide have diabetes, while in Vietnam about 4.5 million people have it, of which about 20% of people with diabetes have eye complications with varying degrees of severity. If not detected and treated early, the lesions of the disease in the fundus will be very severe such as macular edema, retinal hemorrhage, vitreous hemorrhage, retinal detachment... leading to blindness.
1. Causes of Diabetic Retinopathy
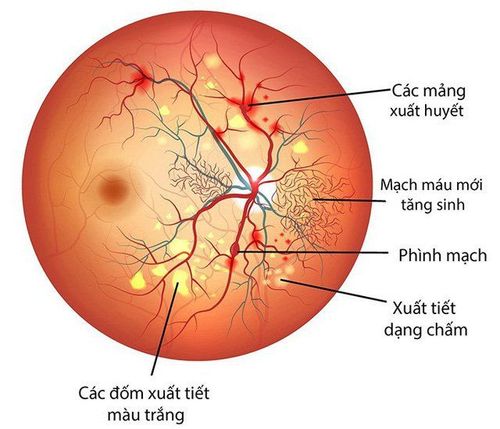
Diabetes causes damage to the blood vessels of all organs in the body, most evident in the microvasculature. In the eye, due to damage to the retinal capillaries, increased vascular permeability, plasma leakage into the retina causes edema. When the capillaries are destroyed, causing blockage and lack of blood to the retina, the body responds by secreting factors that stimulate the growth of new blood vessels (new vessels) to nourish these areas of the retina. However, these blood vessels are fragile and easily broken, causing complications such as vitreous hemorrhage, fibrosis, and retinal detachment.The retina is the light-sensitive part, in which the macula is the center of the retina, the place for the most delicate vision. The effects of diabetes on the retina make the retina severely damaged, severely affecting visual function.
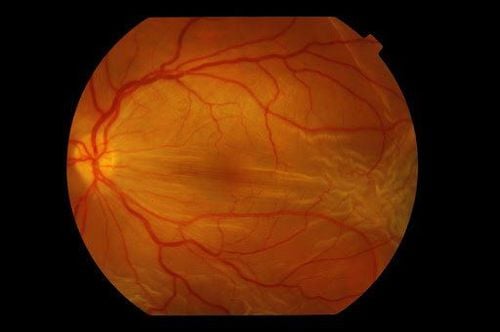
Bệnh võng mạc đái tháo đường
2. Stages of Diabetic Retinopathy
2.1 Background retinopathy: This is an early stage of diabetic retinopathy with lesions such as retinal capillary aneurysm, slight bleeding, stagnation of secretions in the retina, and retinal edema.Pathology at this stage, if it has not invaded the macular area, has not yet caused vision loss. However, patients may feel visual abnormalities such as seeing black spots in front of their eyes, or the sensation of color changes... It is necessary to monitor and treat when there is bad progress, affecting function visual ability.
2.2 Diabetic macular disease: This is the most common cause of vision loss in diabetic patients, especially non-insulin dependent disease, aged 50 - 70 years. The macula (where vision is highest in the eye) is edematous, sometimes cystic, or accompanied by ischemic damage.
Macular edema with hard exudates around the macula
Treatment: When macular disease has appeared with a marked decrease in vision, the patient needs to have an eye exam and laser treatment immediately to restore the macula Soon.
2.3 Pre-proliferative diabetic retinopathy: Damage to the retina at this stage is caused by an abnormal blood supply to the retina, leading to ischemic lesions, hemorrhages, exudates and retinal edema. If these lesions have not invaded the macular region, the patient has not noticed a decrease in vision. Therefore, although the damage to the retina is quite severe, the patient is still not aware, so they often do not go to the doctor and get treatment.
Microaneurysm, exudate, retinal hemorrhage
Treatment: Damage at this stage if it threatens visual function, or causes severe ischemia, requires fluorescence fundusography and laser photocoagulation of the affected areas. injury to prevent complications.
2.4 Proliferative stage diabetic retinopathy. This stage disease is caused by the proliferation of abnormal neovascularization, causing continuous recurrent bleeding, causing organization and pulling of retinal stimulator. The consequences are severe damage to the retina, tear or detachment of the retina leading to blindness. Another common consequence is neovascular glaucoma, chronic pain, extremely difficult to treat.
Treatment: Patients at this stage need emergency laser photocoagulation of the entire retina. The progression of the disease at this stage is very rapid and severe, especially when diabetes is not completely treated.
3. Eye exams for early detection and treatment of diabetic retinopathy
Screening: All patients with diabetes should be screened for early detection of the disease: The examination procedure includes visual acuity testing, pupil dilation for systematic ophthalmoscopy on a microscope. Depending on the stage of the disease and the damage to the retina, the doctor will prescribe treatment or periodically monitor it.Along with it, patients need to be actively treated for diabetes, bringing blood sugar levels back to normal
4. Diabetic retinopathy examination process
General eye exam to assess general eye function Apply pupil dilator for fundus examination Color fundus imaging to identify early lesions If lesions are present, fluorescein angiography and OCT scan for evaluation. The digital fluorescein angiography system allows the detection of abnormal edema, hemorrhage, anemia, and neovascular lesions very accurately. OCT is also an extremely modern method to evaluate the edema and damage of the central retina
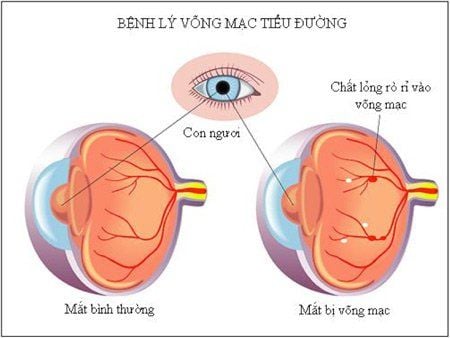
Hình ảnh bệnh võng mạc tiểu đường
5. Treatment methods for diabetic retinopathy depend on the stage of the disease
Retinal laser photocoagulation Intraocular injection of anti-neovascular drugs and anti-macular edema drugs Vitreous resection and retinal detachment to treat late-stage complications Basic and thorough treatment for Diabetic retinopathy is laser retinal photocoagulation.Laser purpose is to destroy abnormal retinal areas, kill new vessels and treat macular and retinal edema. Current common lasers still have disadvantages such as difficulty in controlling laser energy, leading to damage to areas of the retina that do not require treatment, extensive scarring, reduced peripheral vision, and reduced perception. color and night vision. In addition, the laser for each individual nodule makes the treatment time longer, causing a lot of pain for the patient.
Pascal beam laser is the most advanced retinal photocoagulation laser device in the world today, overcoming many disadvantages of common lasers today.
The time of laser effect on retinal tissues is very short, does not cause extensive burns around the laser area, so it helps control the desired effect, causing less damage to the retina around the laser area. In order to form a multinodular beam, the beam laser program has many modes suitable for the anatomical morphology of the macula and retina, thus shortening the treatment time and minimizing the number of treatments. No or very little pain. Minimize complications and side effects of laser. Before, during and after laser treatment, intraocular injection for retinal neovascularization (Avastin, Lucentis), and macular edema (Triamcinolone) are reviewed and indicated for each specific condition. body.
Vitreo-retinal surgery is indicated in the final stage of the disease, cutting off the blood and organizing in the vitreous chamber, treating retinal detachment. however, in the late stages often do not bring good results for visual function. The disease often causes blindness.
6. Other therapeutic applications of Laser Pascal
Central retinal vein occlusion Disease uveitis retinal microvascular malformations and abnormalities, retinal neovascularization Retinal tear not causing retinal detachment Peripheral retinal degeneration with risk of detachment Retinal. Central serous chorioretinopathy SEE MORE
Beware of hypertensive retinopathy What is retinopathy? What are the common types? How dangerous is diabetic retinopathy?