This is an automatically translated article.
The article was professionally consulted with Doctor Phan Diem Doan Ngoc - Department of Obstetrics and Gynecology, Vinmec Central Park International General Hospital.Chronic pelvic pain in women can be a manifestation of gynecological disease with a duration of about 3-6 months. This disease accounts for about 10% of women's gynecological visits and 20-30% of laparoscopy cases. In the case of non-gynecological problems, pain may be caused by gastrointestinal disease, bladder interstitial inflammation, musculoskeletal disease or ectopic pregnancy.
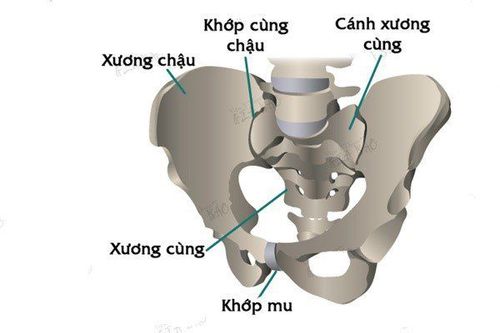
1. Pelvic pain
Pelvic pain is pain in the lowest part of the abdomen and pelvis. In women, pelvic pain can be symptoms arising from the reproductive, urinary, or digestive systems, or from musculoskeletal sources. Depending on the source, pelvic pain can be dull or sharp or intermittent. Pelvic pain can sometimes radiate to areas such as the lower back, buttocks, or thighs. Pelvic pain can be sudden, strong, and short (acute pelvic pain) or long-term (chronic pelvic pain).Chronic pelvic pain can have many causes. However, it can also be a symptom of another disease. If chronic pelvic pain is caused by other medical problems, treating these factors can eliminate the pain. But, in many cases where the cause of chronic pelvic pain may not be identified, the goal of treatment may be to relieve pain and other symptoms to improve quality of life.
Đau vùng xương chậu mãn tính có thể có nhiều nguyên nhân
2. Signs and symptoms
Chronic pelvic pain can be described in many ways such as:Severe and stable pain Intermittent pain Dull pain Sharp or cramping Pain and heaviness deep in the pelvis Other symptoms include:
Pain during intercourse Pain when urinating Pain when sitting for a long time Discomfort may increase after standing for long periods and may be relieved by lying down. The pain can be mild and uncomfortable or it can be so severe that it is impossible to do anything, sleep, or exercise.

Đau xương chậu sẽ xuất hiện các cơn đau âm ỉ, không dồn dập
3. Cause
Chronic pelvic pain is a complex condition that can have many causes. Sometimes, a single disorder can be identified as the cause. However, in other cases, pain may be the result of a medical condition, such as endometriosis and interstitial cystitis, both of which cause chronic pelvic pain. .Some causes of chronic pelvic pain include:
Endometriosis. This is a condition in which tissue from the lining of the uterus grows on the outside of the uterus. These tissues respond to the menstrual cycle, just as the lining of the uterus thickens, breaks down, and bleeds each month, as hormone levels rise or fall. Because it occurs outside the uterus, blood and tissue cannot exit the body through the vagina. Instead, they remain in the abdomen and they can lead to painful cysts and fibrous bands of scar tissue. Musculoskeletal problems. Conditions that affect the bones, joints, and connective tissues (musculoskeletal system) such as myalgia, pelvic floor strains, pubic symphysis (pubic sympathomimetics), or hernias can lead to regional pain recurrent pots. Chronic pelvic inflammatory disease. This can happen if a long-term infection, often sexually transmitted, causes scarring involving the pelvic organs. The rest of the ovary. After surgical removal of the uterus, ovaries, and fallopian tubes, a small piece of an ovary can be accidentally left inside and then develop into a painful cyst. Fibroids. These noncancerous uterine growths can cause pressure or a feeling of heaviness in the lower abdomen. They rarely cause sharp pain unless they are deprived of their blood supply and begin to die (degenerate). Irritable bowel syndrome . Symptoms associated with irritable bowel syndrome such as bloating, constipation, or diarrhea can be a source of pelvic pain and pressure. Bladder pain syndrome (interstitial cystitis). This condition is associated with recurrent pain in the bladder and frequent need to urinate. There may be pelvic pain when the bladder is full, which may improve temporarily after emptying the bladder. Pelvic congestion syndrome. Some doctors believe that varicose veins around the uterus and ovaries can lead to pelvic pain. However, other doctors are less certain that pelvic congestion syndrome is the cause of pelvic pain because most women with enlarged veins in the pelvis have no associated pain. Psychological factors. Depression, chronic stress, or a history of sexual or physical abuse can increase your risk of chronic pelvic pain. Emotional distress makes pain worse, and living with chronic pain contributes to emotional distress. These two factors often become a vicious cycle.
4. Diagnosis
In addition to a detailed interview about your pain history, family history, and some of the symptoms of chronic pelvic pain, tests or exams are needed to confirm a diagnosis.Pelvic examination. This can reveal signs of infection or abnormal growth. Your doctor will examine the painful areas. Let your doctor know if you feel any discomfort during this period, especially if the pain is similar to what you've experienced. Test. During a pelvic exam, your doctor may order labs to check for infections, such as chlamydia or gonorrhea. Your doctor may also order blood tests to check your blood cell counts and a urinalysis to check for urinary tract infections. Supersonic. This test uses high-frequency sound waves to create accurate images of structures in the muscle. This method is especially useful for detecting masses or cysts in the ovaries, uterus, or fallopian tubes. In addition, additional imaging tests such as an abdominal X-ray, computed tomography (CT) scan, or magnetic resonance imaging (MRI) may be used to help detect abnormal structures or growths. Endoscopic. During laparoscopic surgery, your doctor makes a small incision in your abdomen and inserts a thin tube attached to a small camera (endoscope). This method will allow your doctor to view your pelvic organs and check for abnormal tissue or signs of infection. This laparoscopic procedure is particularly useful in detecting endometriosis and chronic pelvic inflammatory disease.
5. Treatment
The goal of chronic pelvic pain treatment is to relieve symptoms and improve quality of life. If your doctor can pinpoint a specific cause, treatment will focus on that cause. However, in cases where a cause cannot be determined, treatment will focus on controlling pain and other symptoms. For many women, the best approach is to combine treatments together for the best results.Medications: Depending on the cause, your doctor may recommend a number of medications to treat it, such as:
Pain relievers. Examples of over-the-counter pain relievers, aspirin, ibuprofen (Advil, Motrin IB), or acetaminophen (Tylenol), can provide partial relief from pelvic pain. Sometimes a doctor's prescription of pain medication is also needed to deal with chronic pain. Some women find that the days they experience pelvic pain can coincide with a specific phase of the menstrual cycle and hormonal changes. When this is the case, birth control pills or other hormonal medications can help relieve pelvic pain (hormonal treatments). Antibiotic. If an infection is the source of the pain, your doctor may prescribe antibiotics. Antidepressants. Certain types of antidepressants may be helpful for chronic pain. Tricyclic antidepressants, such as amitriptyline, nortriptyline (Pamelor), and others, seem to have analgesic as well as antidepressant effects. They can help improve chronic pelvic pain even in women who don't have depression. In addition, there are other treatments to relieve pelvic pain such as: physical therapy - these are stretching exercises, massage and relaxation techniques that help improve chronic pelvic pain, size spinal manipulation - using an implant that blocks nerve pathways so pain signals don't reach the brain, or endoscopic surgery.
Chronic pelvic pain in women is a fairly common disease, but if the cause is not understood and treated early, it will cause risks affecting health and quality of life. Therefore, if there are signs of unusual, intense and prolonged pain, it is necessary to go to the doctor immediately to find out the cause and have a timely treatment plan.
With a system of modern equipment along with a team of highly specialized, experienced doctors, many years of gynecological examination, when performing the basic gynecological examination and screening package at the Hospital Vinmec International General Hospital, customers will receive:
Gynecological examination Gynecological ultrasound transvaginal ultrasound of the uterus and ovaries Transvaginal ultrasound of the breast on both sides Perform tests such as: Treponema pallidum rapid test, Chlamydia rapid test, taking samples for cervical-vaginal cytology, endoscopic staining bacteria (female vaginal fluid), HPV genotype PCR automated system, Urinalysis by automatic machine. The basic gynecological examination and screening package helps customers detect inflammatory diseases early, so that they can be treated easily and inexpensively.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Article referenced source: Mayoclinic.org