This is an automatically translated article.
Chemotherapy is one of the more commonly used treatments for cancer conditions, including breast cancer. This therapy involves the use of drugs to reduce or prevent the risk of the cancer coming back. In addition, they are also used in combination with other methods to increase the effectiveness of cancer treatment for patients.1. When is chemotherapy used?
Currently, chemotherapy is often used for the following specific cases:*After surgery (adjuvant chemotherapy): adjuvant chemotherapy can be used to kill any cancer cells residual or metastatic but undetectable even with imaging. If these cells are not removed, they will thrive and form new tumors elsewhere in the body. In addition, adjuvant chemotherapy can also significantly reduce the risk of breast cancer recurrence in women.
*Pre-surgery (neo-adjuvant chemotherapy): usually given as an injection to shrink tumors and make it easier for doctors to remove them from the body through a less extensive surgery. Therefore, neoadjuvant chemotherapy is mainly used to treat serious cancer conditions that cannot be completely removed by surgery when it is first diagnosed (called locally advanced cancer). ). In addition, performing chemotherapy before the tumor is removed will help the doctor to assess the cancer's response to this method. If the first set of chemotherapy drugs does not shrink the tumor, the patient may have to switch to other drugs that have similar effects. Like adjuvant chemotherapy, neoadjuvant chemotherapy can reduce the risk of breast cancer recurrence for patients.
* Treatment of advanced breast cancer: chemotherapy may be used as a primary treatment for women whose cancer has spread beyond the breast and underarm area. The length of treatment will depend on how well the chemotherapy is working and how well the patient tolerates it.
2. Chemotherapy drugs used for breast cancer patients
As mentioned above, chemotherapy can be given before surgery (neoadjuvant chemotherapy) or after surgery (adjuvant chemotherapy). In most cases of breast cancer, chemotherapy is most effective when several drugs are used in combination.2.1.Adjuvant and neo-adjuvant drugs
Commonly used adjuvant or neo-adjuvant drugs in the treatment of breast cancer include:Anthracyclines, such as doxorubicin (Adriamycin) and epirubicin (Ellence) Taxanes, such as paclitaxel ( Taxol) and docetaxel (Taxotere) 5-fluorouracil (5-FU) or capecitabine Cyclophosphamide (Cytoxan) Carboplatin (Paraplatin) Often, breast cancer patients can take a combination of these 2-3 drugs together. to improve treatment effectiveness.
Trắc nghiệm: Những lầm tưởng và sự thật về ung thư vú
Ung thư vú có tỷ lệ tử vong cao nhất ở nữ giới khiến họ rất lo sợ bản thân mắc phải căn bệnh này. Tuy nhiên, không ít chị em có những hiểu biết thái quá về ung thư vú. Thử sức cùng bài trắc nghiệm sau sẽ giúp bạn loại bỏ được những nghi ngờ không đúng về căn bệnh này.
Bài dịch từ: webmd.com
2.2.Drugs for metastatic breast cancer (advanced breast cancer)
Chemotherapy drugs commonly used to treat metastatic breast cancer include:Taxanes, such as paclitaxel (Taxol), docetaxel (Taxotere), and albumin-bound paclitaxel ( Abraxane) Anthracyclines, eg Doxorubicin, pegylated liposomal doxorubicin and Epirubicin Platinum chemotherapy agents, including cisplatin and carboplatin Vinorelbine (Navelbine) Capecitabine (Xeloda) Gemcitabine (Gemzar) Ixabepilone (Ixempraven) Eribin though Late-stage breast cancer is usually treated with single chemotherapy drugs. However, in some cases it is still possible to use chemotherapy drugs together, such as paclitaxel and gemcitabine. For HER2-positive cancer, one or more drugs that target HER2 may be used along with chemotherapy.

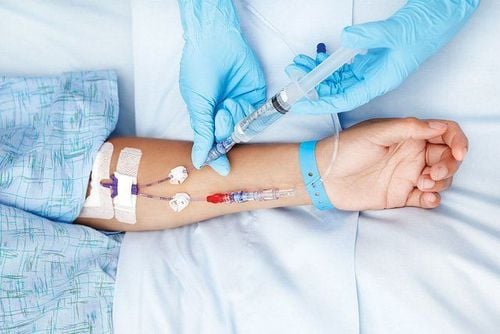
3. How is chemotherapy used?
Chemotherapy drugs for breast cancer are usually given by injection into a vein (IV) within a few minutes or through an intravenous line for a longer time.Intravenous (IV) administration usually requires the use of a central venous catheter (CVC), central venous access device (CVAD), or central line. They are used to get drugs, blood products, nutrients, or fluids into the patient's bloodstream. In addition, they are also used to draw blood for testing.
There are many different types of CVCs available today, the most popular ones are PICC gates and lines. For breast cancer patients, the central line is usually placed on the opposite side of the arm where the lymph nodes have been removed for breast cancer surgery.
Most chemotherapy will be injected in cycles, after which the patient will have a period of rest to recover from the effects of the drug. The longest cycle is from 2-3 weeks. The schedule may vary depending on the medication used. For example, some chemotherapy drugs are given only on the first day of the cycle. In other cases, they may be given for several days in a row or once a week. Then, at the end of the cycle, the chemotherapy schedule is repeated to start the next cycle.
Adjuvant and neo-adjuvant chemotherapy is usually applied for a total of 3-6 months, depending on the drug used by the patient. The length of treatment for terminal breast cancer will depend on how well the drugs work and their side effects on the patient's body.
4. Dosage of chemotherapy
Doctors have found that giving cycles of certain chemotherapy drugs closer together can reduce the risk of cancer coming back and improve survival for some patients. For example, drugs that were originally given every three weeks could be switched to every two weeks. This can apply to both neoadjuvant and adjuvant chemotherapy.However, this therapy can lead to a decrease in blood cell counts, so it is not a safe option for all women. Patients can then have a combination chemotherapy of doxorubicin (Adriamycin) and cyclophosphamide (Cytoxan), followed by weekly paclitaxel (Taxol).
5. Possible side effects of chemotherapy for breast cancer
Chemotherapy drugs can cause certain side effects in breast cancer patients. This also depends on the type and dose of chemotherapy drugs used, as well as the length of treatment. Some of the most common side effects that may occur include:Hair loss Mouth sores Loss of appetite or weight changes Nausea and vomiting Diarrhea Chemotherapy can also affect the blood-forming cells of the bone marrow and leads to:
Increased chance of infection (due to low white blood cell count) Easy bruising or bleeding (due to low blood platelet count) Fatigue (due to low red blood cell count and other reasons) These side effects usually go away after treatment ends. Medications can be used by patients to alleviate the nausea or vomiting that occurs as a result of chemotherapy.
*Changes in menstrual cycle and fertility problems: Changes in the menstrual cycle are a common side effect of chemotherapy, especially for younger women. Early menopause (no more periods) and infertility can be temporary, or permanent. Furthermore, the older a woman is when receiving chemotherapy, the more likely she is to experience menopause or become infertile. This will increase the risk of bone loss and osteoporosis.
Even if your period has stopped during chemotherapy, there is still a chance you can get pregnant. Pregnancy during this time can lead to birth defects in the fetus and interfere with treatment. If you're perimenopausal before breast cancer treatment and are sexually active, it's best to talk to your doctor about using birth control that's right for you. After treatment is complete, women can safely continue to give birth.
*Heart damage: Chemotherapy drugs such as doxorubicin and epirubicin can cause permanent heart damage (cardiomyopathy). The highest risk may occur when these drugs are used for a long time or in high doses. In addition, taking these drugs while you have risk factors for heart failure, such as a family history of heart problems, high blood pressure, and diabetes also contributes to your risk. higher health risks.
In addition, your heart function will be checked through an echocardiogram or MUGA scan before starting these medications. If heart function begins to deteriorate, treatment with these drugs will be stopped temporarily or permanently. However, in some people, signs of heart damage may not appear until several months or years after stopping treatment.
*Nerve damage (neuropathy): many drugs are used to treat breast cancer, including taxanes (docetaxel, paclitaxel, and protein-bound paclitaxel), platinum chemotherapy agents (carboplatin). , cisplatin), vinorelbine, eribulin, and ixabepilone can damage nerves in a patient's hands, arms, and feet or legs. This can cause those areas to become numb, painful, burning, tingling, sensitive to cold or heat, and debilitating. In most cases, these symptoms go away after treatment is stopped, but in some women it can persist or become permanent.
*Hand-foot syndrome: Some chemotherapy drugs, such as capecitabine and liposomal doxorubicin, can irritate the palms and soles. This is called hand-foot syndrome. Initial symptoms include numbness, tingling, and flushing. If it gets worse, the hands and feet can become swollen and cause discomfort, even pain. In addition, the skin may blister, leading to peeling or open sores. To prevent these symptoms, patients can use certain creams or steroids before chemotherapy.
*Cognitive decline after chemotherapy (brain dysfunction): some women treated with chemotherapy for breast cancer may experience a slight decrease in brain function. They may have some lingering problems with concentration and memory.
*Increased risk of leukemia : very rarely certain chemotherapy drugs can cause bone marrow diseases, such as myelodysplastic syndrome, or even acute myeloid leukemia - a leukemia cell cancer. This usually happens within 10 years of treatment.
* Body fatigue: after chemotherapy, many women feel that their bodies are no longer as healthy as before. A number of symptoms may occur, including body aches and mild loss of physical function lasting months to years.
When palliative care is taken along with all other appropriate treatments, people with cancer can feel better and live longer. The palliative care team is made up of doctors, nurses, and other specially trained professionals. The supportive palliative care team aims to improve the quality of life for people with cancer and their families.
At Vinmec International General Hospital, there is a Breast Cancer Screening Package to help detect breast cancer early even when there are no symptoms.
Breast cancer screening package at Vinmec for the following subjects:
Female customers, over 40 years old. Customers wishing to be able to screen for breast cancer Customers are at high risk of cancer – especially customers with a family history of breast cancer. Women of reproductive age, perimenopause and menopause. Women who are having symptoms of breast cancer, such as: breast pain, breast lump, etc. Please make an appointment on the website to be served.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: cancer.org