This is an automatically translated article.
The article was written by MSc Huynh Vuu Khanh Linh - Doctor of Obstetrics and Gynecology, Department of Obstetrics and Gynecology - Vinmec Phu Quoc International General Hospital.A C-section is a cesarean section with an incision in the mother's abdomen and in the uterus. Caesarean section is indicated when it is a safer option for mother and fetus than vaginal delivery.
1. Reasons for having a cesarean section
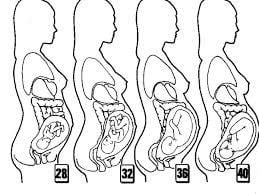
The caesarean section (outside the skin and on the uterus) is located in the lower part of the pregnant woman's abdomen. The incision on the mother's abdomen can be a longitudinal line below the navel or a transverse line above the scapula. The incision in the uterus can be horizontal or vertical. A transverse lower uterine incision is more commonly used because the incision heals well and there is less bleeding. A transverse incision in the lower uterine segment also increases the chance of a vaginal delivery in a subsequent pregnancy. However, the choice of incision is based on the condition of the mother and the fetus.If the woman cannot have a vaginal delivery, the fetus will be removed surgically. Some cesarean sections are planned in advance (elective cesarean section). The other cases are usually an emergency cesarean section due to problems during labor.
Irregular fetal heart rate: Fetal heart rate during labor is a good indicator of fetal response to uterine contractions. Normal fetal heart rate is 120-160 beats/minute. If the fetal heart rate is abnormal, immediate intervention is required: give the pregnant woman oxygen, give fluids, change position (lying on the left side). Cesarean section is indicated if necessary. Abnormal fetal position: the normal position of the fetus is the head position, facing the mother's back. Sometimes the position, position, or position of the fetus is not favorable, making it difficult for a vaginal delivery. Unusual or failed labor. The fetus is too big for the mother's pelvis.

Trường hợp thai nhi quá to so với khung chậu của người mẹ, cần được chỉ định mổ lấy thai
Placental abnormality: placenta previa (placenta covers the hole in the cervix - making it impossible for the fetus to give birth vaginally). Placenta previa can prematurely slough off causing bleeding when the pregnancy is not yet full term. Maternal diseases that can increase the rate of cesarean section such as diabetes, high blood pressure or some other infections. Twins or other multiples. History of previous cesarean section. There are many reasons, the doctor will consider and advise the pregnant woman to continue to monitor vaginal delivery or cesarean section.
2. Risk of cesarean section
Like other surgeries, cesarean section also carries risks.
Bleeding: common due to the uterus after surgery is not good, bleeding from the placenta attaches abnormally, especially in women with a history of previous cesarean section. Bladder and bowel damage. Intrauterine infection, surgical site infection. Urinary tract infection. Urinary retention, difficulty urinating. Bowel obstruction . Thrombosis. The next time a woman becomes pregnant, the risk of having to have a cesarean section continues. However, pregnant women can still monitor vaginal delivery even with old incisions. Vaginal delivery after cesarean section depends on whether the cause of the previous caesarean section exists, whether the incision in the uterus is strong enough to withstand labor contractions, and whether the pregnant woman has any accompanying abnormalities. Vaginal delivery in women with a cesarean section carries a higher risk (uterine rupture) and requires close monitoring.
Nguy cơ nhiễm trùng vết mổ và huyết khối ở phụ nữ mổ đẻ
3. Caesarean section procedure
3.1 Before surgery The obstetrician and the anesthesiologist will advise the pregnant woman and her family about the methods and risks of surgery. Pregnant women and families can ask more questions to better understand this method. The pregnant woman will sign an agreement to consent to the surgery. Pregnant women need to carefully read the commitment and immediately ask the doctor for advice when in doubt. If the pregnant woman wants to have tubal sterilization sterilization (permanent birth control) and meets the conditions prescribed by the Ministry of Health, the pregnant woman will sign an additional commitment for this sterilization surgery. If the pregnant woman has an elective cesarean section, she will fast for 8 hours before the surgery. Pregnant women will inform the medical staff about the drugs and foods they are allergic to. Pregnant women will inform medical staff of the over-the-counter medicines and dietary supplements that they are using. Pregnant women will inform the medical staff about the history of bleeding, history of using anticoagulants. The use of these anticoagulants must be stopped before surgery. Pregnant women may be prescribed drugs that antagonize stomach acid, reduce secretions of the digestive and respiratory tracts. Pregnant women should plan about who will take care of themselves and their baby after surgery. Because after surgery, pregnant women may have pain for the first few days and need someone to take care of the baby. Depending on the specific situation, the Doctor may have other instructions to prepare for the surgery to be safe.
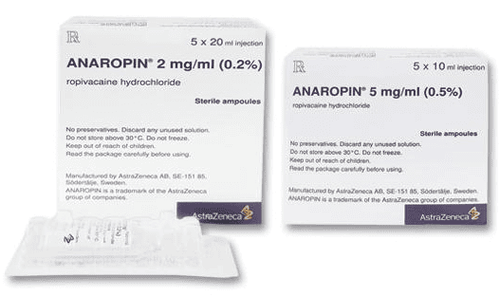
3.2 In surgery The cesarean section is carried out in the operating room, following the principles of sterility and safety in surgery. Prophylactic antibiotics will be used before surgery within 60 minutes. Pregnant women will shower before surgery and wear a hospital gown. Hair will be carefully tied back and the operating room cap will be worn. The pregnant woman was placed intravenously with intravenous fluids, placed a urinary catheter and cleaned before surgery with an antiseptic solution. The abdomen is then carefully covered with a sterile towel. The anesthesiologist will monitor your heart rate, blood pressure, breathing rate, and oxygen saturation throughout the surgery.

Thai phụ được đặt vein truyền dịch trong quá trình phẫu thuật lấy thai nhi
Most pregnant women will be awake during the surgery. Pregnant women will be given spinal anesthesia or epidural anesthesia. At that time, the pregnant woman no longer feels pain from the hip down to the leg but is still awake and can hear and see the baby when the baby is taken out of the womb. However, there are a few situations in which a pregnant woman will be sedated. After the surgeon breaks the amniotic fluid, the fetus is removed. You may feel a little bit of the surgeon's push on your belly when you hold the baby. After the umbilical cord is cut, the surgeon will remove the placenta from the uterus. The anesthesiologist will inject drugs to help the uterus contract and stop bleeding. The uterus and abdominal wall will be sewn up. The skin will be covered with sterile wipes or bio-glue.
3.3 After surgery In the hospital
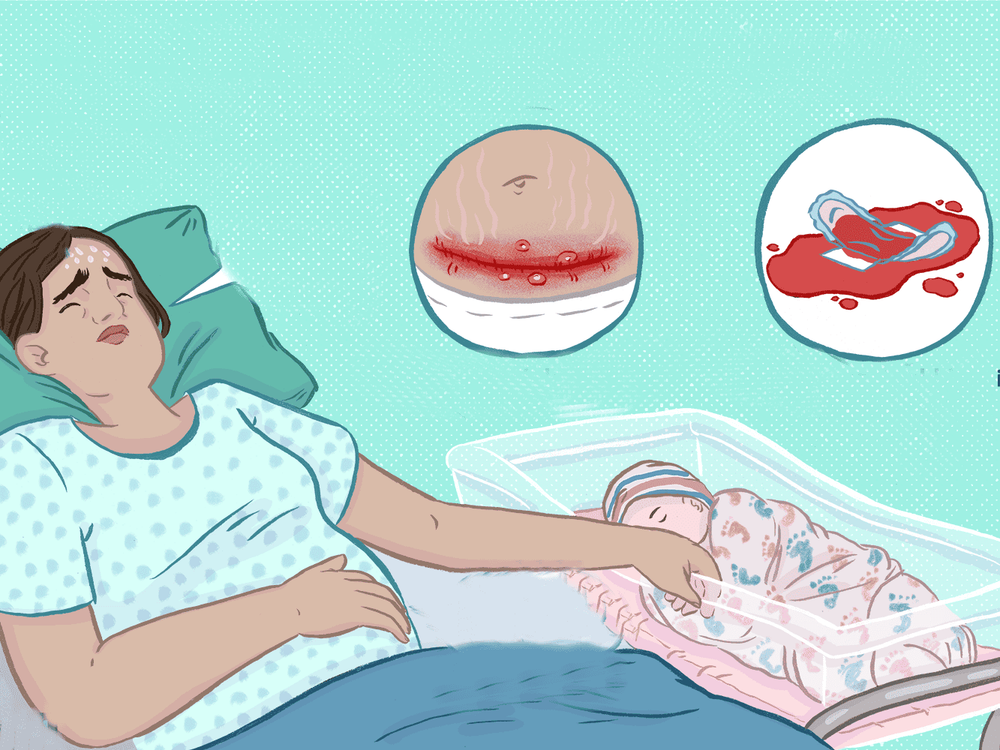
Pregnant women will be monitored postoperatively in the recovery room. Vital indicators such as pulse, blood pressure, breathing rate, degree of contraction of the uterus, vaginal blood, bleeding from incision, urine... Normally, the baby can be returned to the mother after when checked by a pediatrician, weighed after surgery to perform the first feeding. Or the baby can be done skin-to-skin early with the mother in the operating room. Pregnant women can be relieved of postoperative pain by anesthesia of the lumbar squamous muscle at this time. This technique helps pregnant women reduce pain after surgery, mobilize and recover early. After two to six hours of monitoring in the recovery room, the pregnant woman will be transferred to the Inpatient area for customers after cesarean section. Depending on the specific situation, pregnant women can drink water for a few hours after surgery, food should be from thin to solid. The urinary catheter will be removed the day after surgery. Pregnant women will practice urinating and notify the doctor if there are abnormalities, bladder tightness after catheter removal. Pregnant women are encouraged to exercise early to stimulate bowel movements and prevent blood clots. Pregnant women should start with movement in bed, practice walking around the bed and then around the room. Should have relatives beside the pregnant woman to prevent falls.

Sản phụ có thể được ăn thức ăn lỏng sau mổ đẻ
Go home
Pregnant women still use thick tampons, change them often because the fluid is still secreted in the first few days after giving birth/cesarean section. The discharge will change from dark red to brown after a few weeks. Women should not douche, do not use vaginal tampons and abstain from sex in the postpartum period. Pregnant women should also exercise gently, avoid heavy work, carry, drive... Pregnant women can use pain relievers when prescribed by a doctor. Aspirin can increase the risk of bleeding. Follow-up visit 2-3 weeks after surgery. If you have the following signs, you need to see a doctor immediately: Heavy bleeding. Foul vaginal discharge. Abdominal pain a lot. The incision is painful, red, hot, swollen, or bleeding. Footsore. Pregnant women are advised to breastfeed and prevent pregnancy after surgery.
Vinmec International General Hospital offers a Package Maternity Care Program for pregnant women right from the first months of pregnancy with a full range of antenatal care visits, periodical 3D and 4D ultrasounds and routine tests to ensure that the mother is healthy and the fetus is developing comprehensively.
Pregnant women will be consulted and checked for health under the close supervision of experienced and specialized Obstetricians, helping mothers have more knowledge to protect their health during pregnancy as well as reduce reduce complications for mother and child.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.