This is an automatically translated article.
Endometrial hyperplasia, also known as endometrial hyperplasia, is an abnormal proliferation of glands in the endometrium in size and shape that causes the gland/stromal ratio to increase compared to the endometrium. normal endometrium. The main cause is an excess of estrogen or a deficiency of progesterone by the corpus luteum.
1. The concept of endometrial proliferation
Endometrial hyperplasia, also known as endometrial hyperplasia, is an abnormal proliferation of glands in the endometrium in size and shape that causes the gland/stromal ratio to increase compared to the endometrium. normal endometrium.
According to the World Health Organization WHO, endometrial hyperplasia is classified into 4 groups:
typical simple proliferations typical complex proliferations atypical simple proliferations complex proliferations Atypical Such division is based on two main factors: ductal/stromal composition (simple or complex) and the presence of malformed macronuclear cells (typical or atypical). Figure). Simple proliferation means that the ducts are structurally simple and stromal is abundant. Unlike simple, complex proliferation is a condition in which the proliferative glands are dense, crowded, and have very little stroma. The typical concept means that there is no presence of abnormal cells and no structural abnormalities. In contrast, atypical cells are present in the presence of cells with enlarged nuclei, malformation, increased nuclear/cytoplasmic ratio, abnormal shape and size, irregular dark and light chromatin, and abnormal cell division.
It is the presence of large, malformed, atypical cells that are the most important indicator of the risk of progression to endometrial cancer in a woman with endometrial hyperplasia. Specifically, 29% of cases of atypical proliferation will progress to cancer, 8% of cases of typical complex proliferation will progress to endometrial cancer. Meanwhile, only 3% of women in the typical simple prolapse group developed endometrial cancer.
2. Causes of endometrial hyperplasia
When there is no ovulation, there will be no progesterone production, the endometrium will not shed, but continue to grow in response to the amount of estrogen in the body. The cells in the endothelium will crowd together more and more and become abnormal. Therefore, the main cause of endometrial hyperplasia is an excess of estrogen and/or a deficiency of progesterone by the corpus luteum.
In fact, endometrial hyperplasia is more common in the following people:
Puberty Non-ovulatory cycles Irregular periods, especially in relation to polycystic ovary syndrome or infertility infertility . In perimenopause due to a decrease in corpus luteum progesterone levels Postmenopausal women on prolonged high-dose estrogen use Drugs with estrogen-like active ingredients There are also risk factors for increased endometriosis such as:
Caucasian Over 35 years old Never been pregnant Late menopause Early menarche obesity Smoking smoking Personal history of diabetes, thyroid disease, ovarian syndrome Polycystic eggs or gallbladder disease Family history of ovarian, uterine, or colon cancer

Phụ nữ hút thuốc có thể làm tăng nguy cơ mắc tăng sinh nội mạc tử cung
3. Diagnosis of endometrial hyperplasia
Diagnosis of endometrial hyperplasia should be based on clinical symptoms, ultrasound, hysteroscopy and endometrial biopsy.
Symptoms: irregular menstrual cycle, menorrhagia, hypermenorrhea, intermenstrual bleeding Ultrasound: endometrial hyperplasia with increase in endometrial thickness manifested on ultrasound with thickened echo area, ring margin and homogeneity in the uterine cavity. Endometrial thickness at the beginning of the menstrual cycle > 9mm and ≥ 4mm in postmenopausal women. Ultrasound can also detect polycystic ovaries or ovarian cysts.
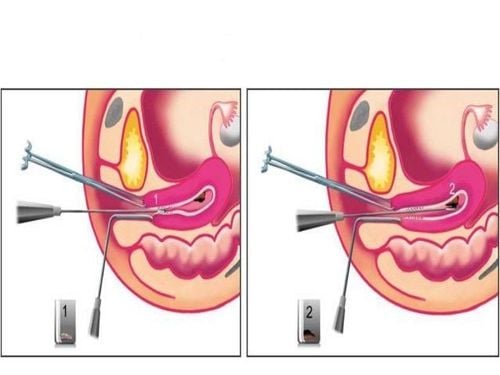
Hysteroscopy shows thickened endometrium, with congested grooves, contour, and irregular thickening of papillae. Hysteroscopy reveals focal or general endometrial hyperplasia, and also helps guide an accurate curettage of endometrial biopsy. Endometrial biopsy to make pathology, to determine the histopathology of the cells to know for sure whether it is cancer or not. Excisional biopsy helps to definitively diagnose endometrial hyperplasia. However, endometrial curettage does not always give an accurate diagnosis. There are some cases of highly differentiated endometrial cancer that is not chromosomally diagnosed (co-presented with atypical endometrial hyperplasia).
4. Endometrial hyperplasia treatment
Treatment of endometrial hyperplasia is based on many factors such as age, clinical symptoms, risk factors,... In which, the decision to treat is mainly based on two factors:
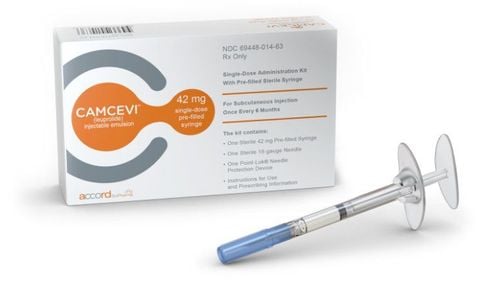
Presence of atypical cells with enlarged, malformed nuclei The desire to maintain fertility of the patient Endometrial hyperplasia at puberty does not require treatment, just dietary adjustment proper care and regular rest. For women of pre-menopausal age, it is necessary to conduct endometrial biopsy for pathological examination. If it is typical simple or complex endometrial hyperplasia, it is necessary to control abnormal uterine bleeding and use progesterone (injectable, oral or vaginal) for 3-6 months. then check again and prevent progression to endometrial cancer. When results show atypical endometrial hyperplasia, the most radical treatment is complete hysterectomy (and two appendages if menopausal), because of the high risk of progression to endometrial cancer. uterine lining. In those who cannot have surgery, progestin therapy can be used.

Phụ nữ mắc tăng sinh nội mạc tử cung nên đến bác sĩ để được thăm khám
Endometrial hyperplasia is a complex disease that affects a woman's health as well as her fertility. Therefore, women need to monitor their menstrual cycle regularly, if the menstrual cycle has any disturbances, they need to see an obstetrician-gynecologist early to have a positive treatment, to avoid a serious disease that will be difficult to treat. difficult and require longer treatment.
In order to help customers detect and treat gynecological diseases early, Vinmec International General Hospital has a package of basic gynecological examination and screening, helping customers detect early infectious diseases and help treat Easy, inexpensive treatment. Screening detects gynecological cancer (cervical cancer) early even when there are no symptoms.
Basic gynecological examination and screening package for female customers, has no age limit and may have the following symptoms:
Abnormal vaginal bleeding Having menstrual problems: irregular menstrual cycle, irregular menstrual cycle Irregular vaginal discharge (smell, different color) Vaginal pain and itching Female clients have several risk factors such as poor personal hygiene, Unsafe sex, abortion,... Female customers have other symptoms such as: Abnormal vaginal discharge, itching, pain in the private area, abnormal vaginal bleeding. In particular, Vinmec now has implemented the ThinPrep Pap Test method, which has created a turning point for the traditional Pap smear method, through membrane-controlled cell transfer technology, which helps to increase the accuracy of the Pap smear. Sensitivity and specificity in detecting precancerous cells, especially adenocarcinoma cells, a type of cancer cell that is difficult to detect.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.