This is an automatically translated article.
The article was written by MSc Nguyen Thi Xuyen - Clinician, Center for Reproductive Support - Vinmec Times City International General Hospital.C-section scar defect - uterine fluid is a matter of great concern in recent times. In recent years, the rate of cesarean section has increased due to professional factors and additional social factors. C-section scar defect is a phenomenon recorded 1-2 years late and maybe 10 years after cesarean section, due to the poor recovery of the scar in the isthmus of the uterus. This can be considered as one of the causes of secondary infertility.
1. What is cesarean scar?
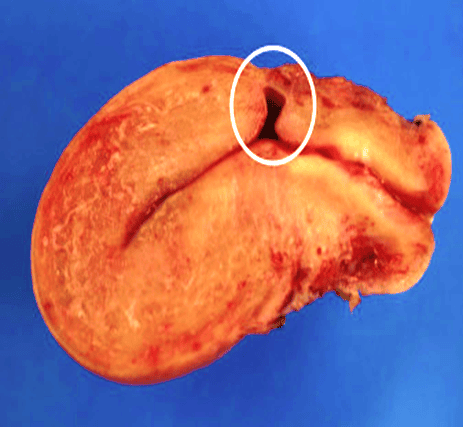
C-section scar defect is the discontinuity of the endometrium, part or all of the anterior wall of the uterine isthmus, which occurs after cesarean section, causing the formation of fluid sacs at the site of the anterior wall of the uterus. the lower part of the uterus, the isthmus, or the upper part of the cervical canal.

2. Scars of cesarean section need to go to the doctor
2.1 Bleeding after period
Also known as heavy menstrual bleeding, bleeding red, black or brown mucus, little discharge, menstrual cycle lasts more than 7 days, bleeding phenomenon after 4 - 5 days after menstruation, corresponding to day 9 - 11 of the cycle, causing discomfort to the patient, due to congestion of the scar mucosa and small polyps, due to accumulation in the defect, dilation of capillaries or loss of the endometrium, surrounding muscles Scar area has poor contractility, reducing menstrual blood flow, causing fluid accumulation.
Besides, bleeding after sex, after vigorous exercise is also mentioned. Usually this phenomenon of menorrhagia does not respond to medical treatment.
2.2 Secondary infertility
Old cesarean scar defect is a difficult problem in the treatment of secondary infertility due to many mechanisms. Presence of varicose veins, lymphocytic infiltration, inferior contracture, and poor contractility of the periscaroid muscle alter the cervical mucus, triggering a chronic inflammatory response that impedes migration. of sperm through the cervical canal, reducing the ability to fertilize or interfere with the implantation of the embryo.
2.3 Uterine fluid retention Often has no clinical manifestations but is detected during mid-menstrual ultrasound or days of menstruation. This issue is of great concern in patients undergoing IVF because embryo transfer is not possible in the middle of the menstrual cycle.
At fertility centers, it is always necessary to find ways to limit fluid retention in the uterus, while the uterine lining is still thick enough, to help increase the success rate of embryo transfer.
2.4 Abdominal pain in the lower abdomen Found in 40% of patients, this is a symptom described by the patient that may be accompanied by pain during intercourse, affecting quality of life. The cause of this symptom may be due to the phenomenon of traction, due to endometriosis at the cesarean scar.
3. Methods used to diagnose cesarean section scar defect
There are many methods of diagnosing cesarean scar defects, each with its own advantages and disadvantages.3.1 Hysterosalpingogram (HSG)

3.2 Magnetic resonance imaging
Rarely used due to high cost3.3 Vaginal ultrasound
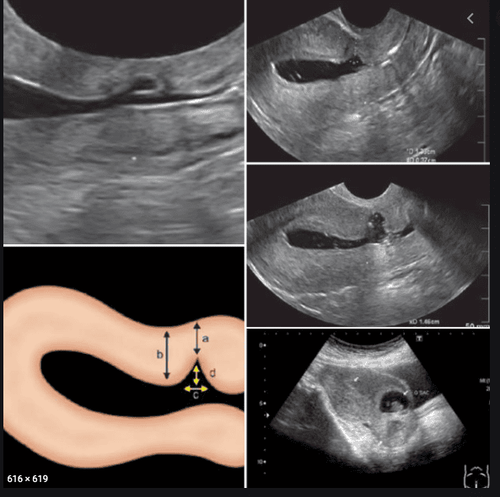
Vaginal ultrasound is the most applied method because it is convenient, cheap and effective compared to other methods.
Vaginal ultrasound is usually done when menstruating or in the middle days of the menstrual cycle, at this time the uterine cavity is secreted to make it easier to observe and measure the size of the defect.
Measurement methods include measuring the upper - lower, left - right, anterior - posterior dimensions and the remaining uterine muscle thickness at the surgical scar site or next to the old surgical scar.
Measure on the vertical line of the uterus in the upper - lower, anterior - posterior dimensions and the remaining uterine muscle thickness.
Measure left - right with cesarean section scars on the horizontal line of the uterus through vaginal ultrasound.
In addition, the distance from the inner orifice of the cervix can be measured to the defect position.
4. Diagnostic hysteroscopy (BTC)
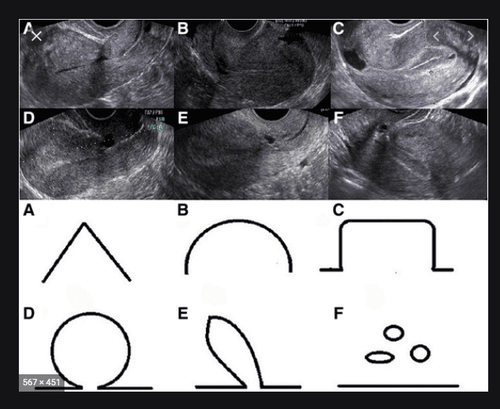
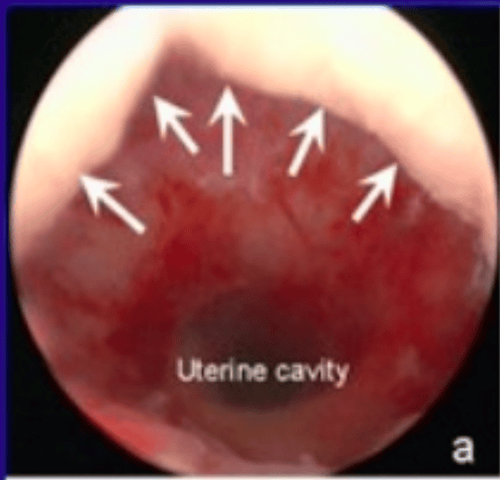
Is the gold standard due to the direct view image. Hysteroscopy also clearly records the entire uterine cavity and the cesarean scar defect area, observes the characteristics of the fluid collection bag, the upper, lower and lower margins of the defect, and endometriosis. or blood pooling at the bottom of the defect area, chronic endometritis can be observed in the defect area.
In addition, hysteroscopy also helps to diagnose the number of defects in patients with a history of multiple cesarean sections.
Hysteroscopy also helps detect causes of blood from the uterus such as submucosal fibroids; Uterine polyps, hyperplasia or atrophy of the uterine lining.
However, hysteroscopy has the weakness of not measuring the remaining uterine muscle thickness, making it difficult to determine the size of the defect, so it needs to be combined with ultrasound for a more effective diagnosis.
5. Methods of treatment of old caesarean scar defects The choice of method of treatment of old caesarean scar defects is completely based on the surgeon's experience and the patient's current condition.
5.1 Hysteroscopy to repair cesarean scar defects is a minimally invasive surgical method using laparoscopic instruments to treat scar defects.
According to Fernandez 2018 endoscopic repair of cesarean section scars improves menorrhagia and heavy bleeding by 65%. In Vietnam, in 2018-2019, author Nguyen Bien Thuy studied the condition of menorrhagia, which improved by 82.4% after scar repair through microscopy.
At Vinmec IVF center, the pregnancy rate after embryo transfer after cesarean section scar treatment by hysteroscopy is 60%.
5.2. Open surgery to treat the defect Open surgery can perform complete removal of the endometrium and reconstruction of the uterus.
5.3 Laparoscopic management of laparotomy Similar to open surgery, the defect is removed by scissors and restored laparoscopically.
5.4 Surgical management of vaginal cesarean scar defect This method is used when determining cesarean section scar defect located low in the uterine isthmus.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.