This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Le Hong Lien - Department of Obstetrics and Gynecology - Vinmec Central Park International General Hospital.Calcification of the mammary gland is common in middle-aged women after the age of 50. Usually mammary calcifications are benign. Mammary calcifications that are irregularly arranged or irregularly shaped (bundle-shaped, markedly bordered) may be a sign of breast cancer. Therefore, it is necessary to pay close attention when the body appears calcified mammary glands.
1. What is calcification?
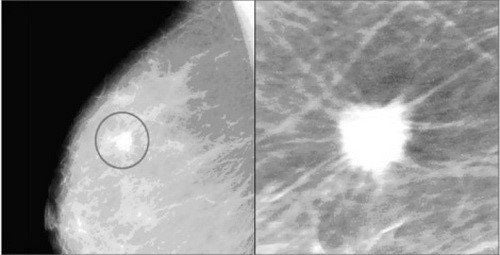
Benign calcifications identified on radiographs are typically round, large, and coarse with smooth margins, more recognizable than malignant calcifications. Calcifications associated with melanoma (as well as many benign calcifications) are usually very small and require the use of a magnifying glass to see better.When a specific cause cannot be found, the description of calcifications should include both their morphology and distribution. It is not necessary to always report obvious benign calcifications. However, they should be reported if the physician reading the film is concerned that other film readers may misinterpret them. Vascular calcification was noted in the results, particularly in women younger than 50 years of age for whom data suggest a potential risk of coronary artery disease.
2. What is mammary gland calcification?
Calcification of the mammary gland is one of the common changes in older women, affecting the physiological functions of breast tissue. Depending on the appearance and size of the calcified nodules, they can be benign or an early sign of breast cancer.Mammary calcification can be defined as the deposition of calcium salts in the female breast tissues. Calcium deposits can be so small that you can't feel them yourself and cause no pain. In general, mammary gland calcifications are usually benign and not much of a concern. However, in certain cases, breast calcifications can be an early sign of breast cancer.
There are 2 types of mammary calcifications that can be detected by mammography:
Large calcifications that appear as large round and white spots on a mammary gland and are randomly dispersed in the breast tissue. Large calcifications are quite common in women over the age of 50, which is a natural sign of breast aging; Microcalcifications or small calcified nodules are very small in size, appearing with many small white spots on mammograms. However, if they appear in clusters or are not limited, small calcified nodules can be a sign of cancer, which needs to be fully examined and diagnosed by a specialist.
3. Causes of mammary gland calcification
Calcification of the mammary gland can be caused by a pre-existing breast injury, leading to tissue damage of the breast or necrosis of fatty tissue. In this case, the amount of calcium deposited increases in the mammary glands; During menopause, women often have breast calcification due to inflammation of the hair follicles on the skin of the breast, vascular calcification in the blood vessels of the breast, and sometimes the involvement of cellular secretions and other substances. cellular debris; Breast cysts, which are filled with small cysts such as lumps in the breast and the presence of fibroadenomas, or benign tumors, or other causes of breast calcification; Disorders associated with ductal dilatation can block or obstruct the milk ducts, leading to increased intraluminal inflammation and calcification. Mastitis or infection of the breast tissues can also lead to increased calcium deposition in the breast tissues; Treatments, such as radiation therapy for breast cancer, can sometimes lead to increased calcification in the breast;
Additional tests may include mammogram with magnification of the calcified areas of the mammary gland, or even biopsy to determine the nature of the calcium deposits, images used to Comparison of calcium deposition patterns in breast tissues.
4. Treatment of calcified mammary glands
If mammary gland calcifications are benign: They are harmless and do not require treatment. You should have a checkup 6 months later to determine if the calcium deposits have changed in appearance or are stable. If nothing changes, your doctor will recommend an annual mammogram to monitor for ongoing mammary calcifications. Besides, you also need to save the previous breast examination records to compare and determine the extent of growth in size and number of mammary gland calcifications; If breast calcification is “probably benign”: This means there is a very low risk of cancer. However you should do another test after 6 months to determine if the deposits have changed in shape or are stable. If nothing changes, doctors usually recommend yearly X-rays for follow-up; If breast calcification is “suspicious”: May be benign, but may also be a sign of cancer. So with this type of breast calcification, your doctor will ask you to do a biopsy to better understand them. If the test results show signs of cancer, the patient will be recommended treatment with radiation, chemotherapy or even surgery to remove the breast. Indicated biopsy sampling methods:Procedural sampling: The doctor will rely on the results of the mammogram and ultrasound to perform this procedure and mark it. Then, a small piece of breast tissue is removed from that area under general anesthesia in a hospital operating room. Finally, the biopsy sample is sent for examination in the pathology laboratory; Needle core biopsy: This procedure is also done frequently. The surgeon cuts out small pieces of tissue with a small, hollow needle with the help of a computer-guided device. The patient is under local anesthesia and does not require surgery, then the removed tissue sample is sent to the pathology laboratory for examination. Breast biopsy with vacuum-assisted suction under Stereotactic positioning: This technique uses a large biopsy needle with a size of 12 G or more, combined with vacuum suction, so it helps to get more specimens, thereby increasing the probability of success. In addition, this technique is also less invasive than the open biopsy method: The incision site does not require any recovery stitches, does not require special care, and the patient can return to normal daily life right away. tomorrow. In addition, the placement of markers to mark the intervention site is carried out right in the procedure to help manage the lesions after the test results are more favorable. This is the most modern technique today, being deployed by Vinmec Times City (Hanoi) and very few hospitals in Vietnam.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














