This is an automatically translated article.
Langerhans histiocytosis (LCH) occurs due to the overgrowth of Langerhans cells and leads to tissue damage, inflammation with multi-organ symptoms. The disease is common in young children and children in the early stages of adulthood, so parents need to be aware and be alert to some conditions such as prolonged impetigo, because it can be a symptom of the disease. Langerhans cells.
1. What is Langerhans histiocytosis?
In the body, myeloid cells develop into monocytes in the bone marrow, then migrate to organs and differentiate into Langerhans cells, also known as dermal dendritic mononuclear cells. The function of this cell type is to present antigens to T lymphocytes, which play an important role in protecting the body from pathogens such as viruses, bacteria, and other foreign invaders.
Langerhans cell histiocytosis occurs due to the overgrowth and abnormality of Langerhans cells, instead of the body's protective role, the overgrowth of this cell type causes damage to the skin, bone tissue. , hematopoietic system, lung... The disease is common in young children and children in early adulthood, the incidence rate at the age of less than 15 years is 0.7 - 4.1/1000000 and in humans Maturity is 1-2/1000000. The disease has a good prognosis when the patient is more than 2 years old and only affects one of the organs such as lymph nodes, skin or bones. In contrast, the risk of disease progression and mortality increases in patients younger than 2 years of age and multi-organ involvement.
Currently, the specific cause of the disease has not been identified, but some factors increase the risk of disease such as cramped living environment, parents exposed to metal, family members with a history of the disease. Having cancer, thyroid disease, pregnant women with infections before and after giving birth increase the risk of disease when the baby is born.
Bệnh mô bào Langerhans dẫn đến các tổn thương mô, viêm với các triệu chứng tại nhiều cơ quan
2. Diagnosis of Langerhan's histiocytosis
2.1. Clinical diagnosis Symptoms caused by Langerhans histiocytosis depend on the location and extent of involvement, and damage can occur in multiple organs. Some symptoms are as follows:
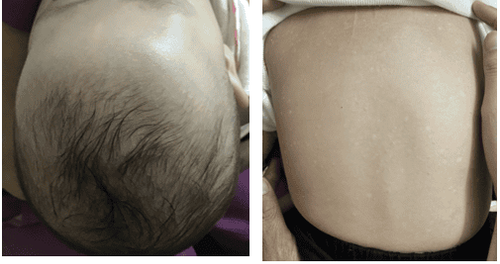
Bone damage: Found in 80% of patients, in which the most common are the ribs, jawbone, skull bone, spine, pelvis, arm bone, thigh bone, surrounding bone. ear and orbital bones. Patients will appear pain at the site of bone damage, soft tissue swelling and lead to secondary symptoms such as otitis media, recurrent mastoiditis, protrusion due to orbital bone damage, fracture. spontaneously due to bone loss, kyphosis due to tumor compressing the vertebrae or due to vertebrae injury... Skin and nail damage: Usually occurs in the scalp, face, buttocks, trunk and fold area. The lesions that occur may be exfoliative, firm yellow or brown edematous and centrally located or widespread, purpura papules, which may have a oozing appearance resembling seborrheic dermatitis. Scalp lesions in young children with Langerhans' cell histiocytosis confuse many parents with children with impetigo, which prolongs the time to detect the disease and aggravates the condition, affecting the effectiveness of treatment. . Injury to liver, spleen, bone marrow: Patients often present with symptoms such as thrombocytopenia, anemia, jaundice, hepatomegaly, splenomegaly, edema or ascites, infection and recurrent fever. perform regularly. Lung damage: Causes symptoms such as dry cough, pneumothorax (difficulty breathing, chest pain, pale skin) and rapid breathing, difficulty breathing... Central nervous system damage: Patients often appear symptoms such as difficulty speaking, loss of balance, difficulty walking, headaches, vision loss, behavioral changes, and memory loss.
Triệu chứng gây ra bởi bệnh mô bào Langerhans phụ thuộc vào vị trí và mức độ liên quan
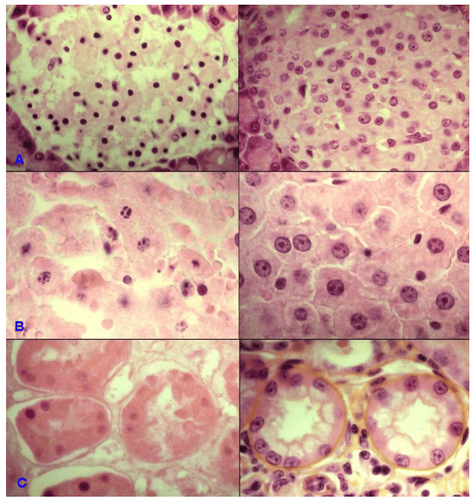
2.2. Laboratory diagnosis Langerhans histiocytosis is a malignancy, so the diagnosis should be based on the results of the following laboratory tests:
Imaging tests:
X-ray of bones: The results show an image of a bone defect or a possible fracture; MRI of the brain and spine showed damage to the bones of the skull and spine; X-ray of the heart and lungs to identify infiltrative nodules with unknown boundaries, pneumothorax; Ultrasound identifies damage to organs such as spleen, abdomen, lymph nodes, liver; Bone scintigraphy: Identify the defect or increase radioactivity at the injured bone site; Whole body PET/CT scan with 18F-FDG before treatment to identify primary tumor, diagnose disease stage and maintain this test during treatment to monitor response to treatment, assess evaluate the risk of disease recurrence or the risk of metastasis. Cell test:
Skin prick test: To determine the increase in the number of retinal cells; Peripheral blood count: Usually results in non-iron deficiency anemia, accompanied by a decrease in platelet count below 100g/l, neutrophil count less than 1.5g/l; Myelogram: Shows many histiocytic cells in the bone marrow and the marrow is not hypoplastic. Biochemical tests:
Liver enzymes GPT, GOT increased; Decrease protein and blood albumin; Pituitary hormone and antidiuretic hormone may decrease; Decreased urine density, protein or red blood cells, white blood cells in urine... Genetic mutation test: May appear mutations in BRAF, MAP2K1, RAS, ARAF genes.
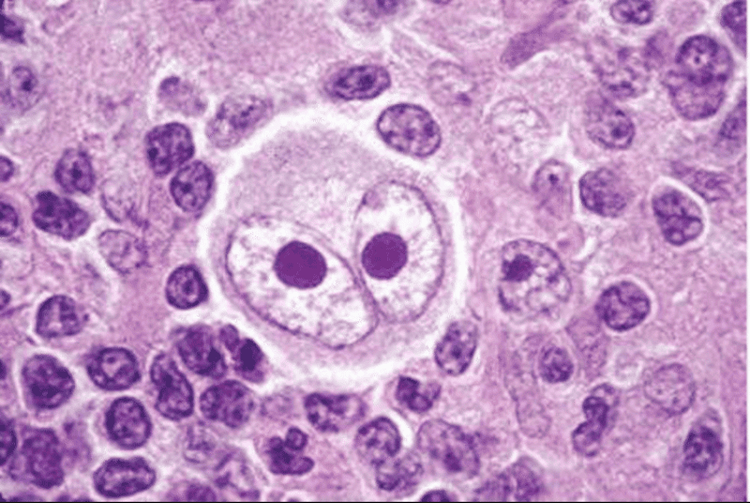
Histopathology: Considered as the gold standard to help diagnose the disease, the results show histopathological images of Langerhans' histiocytosis at the site of tumor biopsy lesion.
Diagnosis is based on clinical symptoms and results of laboratory tests. In addition, the disease is classified into two subgroups as follows:
The disease only causes damage to one of the organs such as bones, skin, lungs, lymph nodes or central nervous system. This group accounts for about 55 - 65%; The disease affects many organs, accounting for 35-45%, of which high-risk organs include spleen, hematopoietic system and liver.
3. Beware of Langerhans histiocytosis (LCH) in children with persistent impetigo
Dendritic mononuclear cells exist in many organs in the body, so people with Langerhans histiocytosis may have symptoms in one or more different organs. In cases where the disease begins with symptoms in the scalp, especially in young children, parents confuse them with children with impetigo. The initial symptoms are the appearance of patches of impetigo, after peeling off again, new episodes, causing itching and bleeding when scratched. If the disease is not detected and treated early, it will lead to damage to other organs such as liver, bones, diabetes insipidus, hemorrhagic rash...
So in the case of children showing similar symptoms At first, parents need to pay attention to monitor the condition and take the child to medical facilities for examination, diagnosis and treatment as soon as possible.
Bệnh mô bào Langerhans là bệnh lý ác tính
4. Treatment of Langerhans histiocytosis
The treatment regimen depends on the condition and extent of spread, damage to the organs and is based on the following principles:
Supportive treatment through hygiene measures to help limit damage to the skin , teeth, ears. Drug treatment: cytotoxic drugs (Mercaptopurine, Vinblastine), corticosteroids (prenisolone, methylprednisolone). The treatment course consists of an attack phase and a maintenance phase, in which the offensive treatment lasts about 6 weeks and 18 weeks for maintenance treatment. Research by scientists shows that 80% of children with Langerhans histiocytosis respond well to aggressive treatments and 81.2% of children with the disease are assessed as having a good response after completing the treatment course. A common side effect during treatment is agranulocytosis and red blood cell count, but these side effects go away after treatment. Some patients are treated with stem cell transplantation, radiation therapy in case other methods fail. Thus, langerhans histiocytosis is a dangerous malignancy and causes symptoms similar to impetigo in children with the disease. Therefore, in the case of a child with impetigo but not being cured by dermatology, parents need to take the child to a medical facility for a general examination in order to detect early and take effective measures to treat the disease. .
Currently, the Pediatrics Department at Vinmec International General Hospital is trusted by many parents to examine the diseases that babies and children have. Vinmec brings satisfaction to customers and is highly appreciated by industry experts by:
Gathering a team of leading pediatricians: including leading experts with high professional qualifications ( professor, associate professor, doctorate, master), experienced, worked at major hospitals such as Bach Mai, 108... The doctors are well-trained, professional, conscientious - understanding and understanding young psychology. In addition to domestic pediatric specialists, the Department of Pediatrics also has the participation of foreign experts (Japan, Singapore, Australia, USA) who are always pioneers in applying the latest and most effective treatment regimens. . Comprehensive services: In the field of Pediatrics, Vinmec provides a series of continuous medical examination and treatment services from Newborn to Pediatric and Vaccine,... according to international standards to help parents take care of their baby's health from birth to childhood. Advanced techniques: Vinmec has successfully deployed many specialized techniques to make the treatment of difficult diseases in Pediatrics more effective: neurosurgery - skull surgery, stem cell transplantation blood in cancer treatment. Professional care: In addition to understanding children's psychology, Vinmec also pays special attention to the children's play space, helping them to play comfortably and get used to the hospital's environment, cooperate in treatment, improve the efficiency of medical treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.