This is an automatically translated article.
Posted by Master, Doctor Tran Quynh Trang - Doctor of Biochemistry Laboratory - Laboratory Department - Vinmec Times City International Hospital
When your immune system attacks the thyroid, it usually targets thyroglobulin. This causes it to produce antithyroglobulin (anti-TG) antibodies. From there, your doctor may order an antithyroglobulin antibody test (anti-TG test) to check the levels of these antibodies in your blood. High levels may indicate an autoimmune condition.
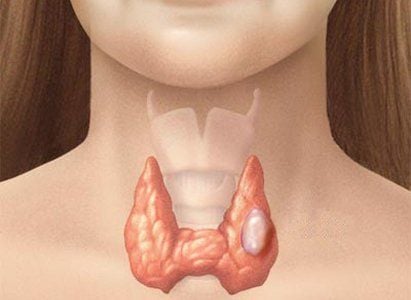
The thyroid gland is an important endocrine gland, shaped like a horseshoe, located in the front of the neck, secreting endocrine substances that play a role in regulating the development of organs, promoting the activity and maturation of all cells. cell. Thyroid dysfunction can cause hyperthyroidism, benign thyroid nodules, and thyroid cancer. The thyroid gland makes a number of different proteins, including thyroglobulin, which uses thyroglobulin to make active thyroid hormones. In the presence of an autoimmune condition, the production of thyroglobulin is disrupted. An autoimmune condition occurs when your immune system produces antibodies that attack your own healthy cells. When your immune system attacks the thyroid, it usually targets thyroglobulin. This causes it to produce antithyroglobulin (anti-TG) antibodies. Your doctor may order an antithyroglobulin antibody test (anti-TG test) to check the levels of these antibodies in your blood. High levels may indicate an autoimmune condition.
Thyroglobulin (anti - TG) antibody is a type G immunoglobulin and a common marker for thyroid autoimmune. Clinical practice has shown that anti-TG is not as useful as anti-TPO in predicting thyroid dysfunction, however anti-TG is found more frequently in differentiated thyroid cancer (DTC). ) and quantifiable, used to monitor recurrence or persistence of DTC. Recent studies suggest a role for preoperative anti-TG in predicting DTC in thyroid nodules and reflecting adverse or prognostic features of the tumor, including lymph node metastasis, but this remains much controversy. Anti-TG after surgery can act as a biomarker for residual thyroid tissue, so monitoring anti-TG levels is useful to predict cancer recurrence in patients. DTC. Differentiated thyroid cancer (DTC) is the most common endocrine cancer, with an increasing incidence worldwide. DTC is found in 7% to 15% of patients with thyroid nodules and it has a good prognosis. The most common type of DTC is papillary thyroid cancer (PTC), which accounts for more than 90% of thyroid cancers, while follicular thyroid cancer is less common, accounting for 7% to 8% cases of thyroid cancer (Korea). Partial thyroidectomy or total thyroidectomy is generally the treatment of choice.
Serum thyroglonulin (TG) is the most sensitive biomarker of TDC after total thyroidectomy and radioactive iodine (RI: ). TG levels can be affected by the presence of Anti-TG antibodies, which can falsely reduce TG levels. Therefore, current cancer management guidelines require concurrent anti-TG testing.
There are many thyroid-related antibodies located in or around the follicular cells including TPO (Thyroid peroxidase)), TSH (Thyroid-stimulating hormone), TG...Gland-related antibodies Thyroid is often associated with autoimmune thyroid diseases such as: anti-TPO, anti-TG indicates Hashimoto's thyroiditis, TSH receptor antibodies indicate Graves' disease.
The anti-TG antibody was the first antibody found in patients with autoimmune thyroid disease (AITD) described by Doniach and Roitt in 1956. Most anti-TG is classified as immunoglobulin G. (IgG), although some are IgA. It is an intracystic antibody that can bind to immune cells and antigens with or without tissue destruction. Mass destruction of the thyroid causes structural changes in the TG, leading to the production of antibodies against TG. The primary T-cell epithelium on the TG requires iodization for self-recognition T cells. This explains the higher prevalence of positive anti-TG levels in patients with excessive iodine intake. However, high levels of TG in the blood do not necessarily produce antibodies. Anti-TG levels depend on the duration of antigen exposure. There are nearly 40 TG epithelium, of which only a few are immunogenic. Anti-TG itself does not damage thyroid cells and it does not immobilize complement because the epithelium is too widely spaced to allow cross-linking.
Many studies have shown that anti-TG plays a role in the relationship between autoimmune thyroiditis and thyroid cancer. The prevalence of anti-TG in patients with DTC is approximately 1.5 times higher than in the general population with benign tumors.
A study retrospectively evaluated a total of 2088 patients with fine needle aspiration (FNA) thyroid nodules and found that thyroid cancer was significantly associated with anti-TG positivity. A similar result was studied by Vasileiadis et al, who found that in patients undergoing total thyroidectomy for any reason, preoperative quantitative testing showed anti-TG in Malignant patients increased more than benign patients (38.2% vs 19.8%). In another study of 2,562 patients with FNA histopathology (FNAC), the cytology of suspicion was found to be higher in anti-TG-positive patients than in patients without anti-TG. 9.4% vs 5.7%), and anti-TG is a risk factor for thyroid cancer. Hosseini et al grouped patients according to the degree of anti-TG and found that the incidence of malignancy was higher in the anti-TG positive group (65.38% vs 50.42%). Qin el al also grouped patients according to anti-TG levels (0.4, 11, 40, 100, and 500 IU/mL), and found that the frequency of DTCs was significantly higher in the high TgAb groups (≥ 100 IU/mL). /mL) compared with the low TgAb groups (<100 IU/mL). In addition to its role in cancer monitoring and treatment, anti-TG testing may be ordered when the following symptoms are present:
Fatigue Unexplained weight gain Constipation Dry skin Goiter Or in the following cases monitor cancer recurrence. Patients with hypothyroidism The anti-TG test is useful in diagnosing autoimmune thyroid diseases: Hashimoto's disease, postpartum thyroiditis, neonatal hypothyroidism, and Grave's disease.
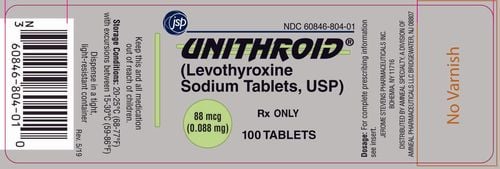
Reference value: < 115 IU/mL
Reference value applies to all ages. Reference values may vary from laboratory to laboratory.

Tg is not secreted into the systemic circulation under normal circumstances. However, follicular destruction due to inflammation (thyroiditis and autoimmune hypothyroidism), hemorrhage (nodular goiter), or rapid growth of disturbed thyroid tissue as may be seen in Graves' disease or Thyroid tumors are of follicular cell origin, which can lead to leakage of Tg into the blood stream. This leads to the formation of autoantibodies to Tg (anti-Tg) in some individuals. The same process can also lead to exposure to other "hidden" thyroid antigens from the immune system, leading to the formation of autoantibodies to other thyroid antigens, especially peroxidase thyroid gland (TPO) (anti-TPO).
Since anti-Tg and anti-TPO autoantibodies are observed most frequently in autoimmune thyroiditis (Hashimoto's disease), they were initially considered to be potentially pathogenic in this disorder. However, today's consensus holds that they are merely signs of disease. It is felt that the presence of competent immune cells at the site of thyroid tissue destruction in simple autoimmune thyroiditis causes the patient to form autoantibodies to thyroid antigens. hidden armor.
In individuals with autoimmune hypothyroidism, 30% to 50% will have detectable anti-Tg autoantibodies, while 50% to 90% will have detectable anti-TPO autoantibodies. In Graves' disease, both autoantibodies are observed in approximately half.
The quantitative antithyroperoxidase (TPO) test has higher sensitivity and equal specificity with the antithyroglobulin (anti-Tg) test in the diagnosis of autoimmune thyroid disease. Therefore, anti-Tg levels should only be measured if anti-TPO is negative, but clinical suspicion of autoimmune thyroid disease is high. The detection of significant titers of anti-Tg or anti-TPO autoantibodies is evidence supporting the diagnosis of Graves' disease in patients with thyrotoxicosis. However, the measurement of pathogenic antithyrotropin (thyroid-stimulating hormone) receptor antibodies is by binding test (THYRO/Thyrotropin Receptor Antibody, Serum) or immunoassay (TSI/Thyroid-Stimulating Immunoglobulin, Serum) is the preferred method to confirm Graves' disease in atypical cases and in exceptional clinical circumstances.
A positive thyroid autoantibody level in patients with normal or slightly elevated serum thyrotropin levels predicts future development of deeper hypothyroidism.
Patients with postpartum thyroiditis with persistently elevated thyroid autoantibodies are likely to have permanent hypothyroidism.
In the case of neonatal hypothyroidism, detection of anti-TPO or anti-Tg in the infant suggests transplacental antibody transfer, especially if the mother has a history of autoimmune thyroiditis or autoantibodies. detectable thyroid gland. Neonatal hypothyroidism may be transient in these cases.
The antithyroglobulin (anti-Tg) and antithyroid peroxidase (anti-TPO) values determined by different methods can differ significantly and cannot be directly compared with each other. Comparison of anti-Tg and anti-TPO values from different methods may lead to implausible clinical interpretation.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
1. Hori M, Katanoda K. Morphological distribution of thyroid cancer from Cancer Incidence in Five Continents Vol. X. Jpn J Clin Oncol. 2015;45:1182. [PubMed] [Google Scholar]
2. For BY, Choi HS, Park YJ, et al. Changes in the clinicopathological characteristics and outcomes of thyroid cancer in Korea over the past four decades. Thyroid. 2013;23:797–804. [PMC free article] [PubMed] [Google Scholar]
3. Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1–133. [PMC free article] [PubMed] [Google Scholar]