This is an automatically translated article.
The article was professionally consulted by Specialist Doctor I Nguyen Xuan Tinh - Anesthesiologist - Resuscitation - General Surgery Department - Vinmec Phu Quoc International General HospitalAnesthesia for traumatic brain injury surgery is the effect of drugs on the brain and total loss of sensation. Anesthesia is usually indicated for the following cases: epidural hematoma, skull concave, skull contusion, intracerebral hematoma... In traumatic brain injury surgery, endotracheal anesthesia is often applied.
1. What is the role of anesthesia in traumatic brain injury surgery?
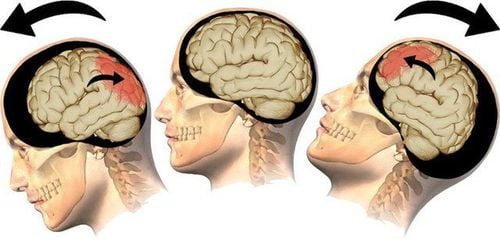
Traumatic brain injury is defined as a blow to the head or trauma that penetrates the skull that disrupts the normal function of the brain. Traumatic brain injury can occur when the head is hit suddenly and sharply with an object, or when an object penetrates the skull and enters brain tissue. There are many types of injuries that require emergency surgery to ensure patient safety such as: skull subsidence, epidural hematoma, brain contusion...
Anesthesia for traumatic brain injury surgery is the effect of the drug on the brain and loss of sensation in the whole body. The drug can be injected through a vein or given to the patient to smell the anesthetic through the airway. With anesthesia, the patient will not know anything and no longer feel pain during surgery, not knowing how and when the surgery happened. Anesthesia in traumatic brain injury surgery is usually applied general anesthesia with intubation for the purpose of breathing control during surgery and resuscitation after surgery. Ensure that the surgery goes smoothly, avoid secondary injuries and maintain good resuscitation in the face of abnormal situations during surgery such as a lot of blood loss, severe cerebral edema...
2. Indications and contraindications
2.1. Indications Epidural hematoma: Usually caused by cortical vein or meningeal artery tear, can be combined with collision, contusion of brain tissue to form intracranial and epidural hematoma. Hematoma surgery. Acute subdural hematoma: Hematoma located between the medial surface of the dura and the cerebral cortex, usually due to tearing of the bridging veins. Surgery to decompress and remove the hematoma. Subacute and chronic subdural hematomas: Craniotomy to drain the hematoma Cranial depression, concave skull: Surgery to lift concave, sunken skull Open head injury: Traumatic brain injury with communication between structures structure in the skull with the external environment. Surgical removal of foreign bodies, dural patching Brain contusion, intracerebral hematoma: Injury to brain cells with hemorrhage. Brain contusions are often seen in the cranial or frontal lobes, because the brain touches the bony ridges of this area. Or a blood clot in the brain tissue itself. Surgical decompression and collection of hematoma 2.2. Contraindications Patients who do not agree: For all indications for surgery, the patient is agreed to agree to cooperate in performing surgery. To ensure liability as well as rare incidents if any occur. In case the patient disagrees for any reason, the doctor only has the right to advise cooperation, not to force it. Insufficient means of resuscitation: In surgical conditions, there are not enough equipment and facilities for recovery, not conducted. Avoid the case that the disease progresses badly, and there are no abnormalities during the implementation. Insufficient means of resuscitation is difficult to ensure a complete operation, the patient may not wake up after anesthesia. Not proficient in technique: The surgeon must be a skilled professional who can apply many different techniques to promptly change the patient's health status during surgery.
3. Anesthesia in traumatic brain injury surgery
3.1. Pre-anesthesia Severe traumatic brain injury: at this time, pre-anesthesia should not be performed due to the risk of respiratory failure. In addition, induction of endotracheal intubation must be performed quickly first, in order to control breathing and airway. Mild trauma: this stage can perform pre-anesthesia applying sedation. The airway and breathing should be continuously monitored while the induction of anesthesia begins. Injury to the brain at the level of agitation: initiate anesthesia and intubate immediately, because pre-anesthesia is almost ineffective at this time. 3.2. Local anesthesia Local anesthesia is often indicated in rare cases of traumatic brain injury in the following conditions:
Brain damage: chronic hematoma, or skull depression, skull concave, no laceration of the cerebral veins. Perception: the patient agrees to cooperate, without agitation. Surgeon agreed and indicated. 3.3. Intubation anesthesia 3.3.1. Induction of anesthesia An intubated endotracheal tube can be difficult due to structural evaluation, the impact of trauma, and the required orientation and position. At this point, the head and neck need to be kept straight on the axis during placement. In case there are signs of suspected injury in the cervical vertebrae, there should be an assistant in the placement of the tracheal tube, a head holder and a shoulder holder to straighten the axis.
Patients should be checked stomach, avoid reflux during induction of anesthesia rapid intubation combined with drugs used to induce anesthesia will be better for severe trauma. Propofol has the effect of slowing down the activity of the brain and nervous system, should only be used with mild traumatic brain injury, because this anesthetic has a high risk of lowering blood pressure. Anesthesia Ketamine is indicated for patients with multiple injuries and low blood pressure. Depolarizing succinylcholine muscle relaxants are indicated for suspected difficult intubation. The non-depolarizing esmeron muscle relaxant allows for rapid induction of anesthesia at doses ≥1mg/kg.
Avoid hypoxia, low blood pressure or excessive increase in blood pressure during induction of anesthesia. The phenomenon of rapid increase in blood pressure, accompanied by increased cranial pressure, or occurs when intubation is intubated. The main reason is because the patient has not slept deeply, the neck and shoulder muscles have not been fully relaxed, the impact of endotracheal intubation is strong and prolonged, causing the body to react.
Do not insert an endotracheal tube or nasogastric tube during a skull base fracture, because of the risk of brain tissue damage from the fracture lines.

The use of volatile drugs should be limited to high doses, and especially for patients with acute cerebral edema should be used at low doses < 1 MAC. The drug can be used after artificial ventilation, can also be used after the skull is opened.
Make sure to relax enough, supplement pain relievers, sleeping pills to avoid coughing, stretching or breathing heavily during surgery.
If brain edema is severe enough, it can lead to dangerous problems:
Hemodynamics It is necessary to maintain the initial blood pressure (when the skull is not open). During surgery, the blood pressure gradually decreased mainly due to lack of circulation, while the sudden drop in blood pressure was easy due to air embolism and damage to the sinuses and cerebral veins.
Ventilation Condition of normal ventilation: The volume of air to be circulated is 8 to 10 ml/kg, the maintenance frequency is 12 to 14 for the purpose of keeping the final CO2 concentration stable at about 35 mmHg, SpO2 is above 95%.
Avoid brain edema during surgery Apply 20% Mannitol type 0.5 to 1 gram/kg, used 20 to 30 minutes before craniotomy. Only used when trauma is accompanied by severe cerebral edema and over a large area.
3.3.3. Response to maintaining anesthesia Blood loss It is difficult to predict this factor because the amount of blood loss can seep around the surgical site. In particular, for children, even small scalp injuries are prone to this incident. Most surgeries to remove the hematoma will open up a large area of the skull, requiring a blood transfusion. When the patient shows signs of damage to the sinus area, it is advisable to carefully apply 2 or more lines for the purpose of blood transfusion and infusion.
Air embolism This symptom is common in the case of sinus and venous injury or excessive bleeding. Continuous monitoring of the final exhalation carbon dioxide concentration will easily detect this condition. The surgeon performing the surgery should immediately seal the bleeding site, place the patient in a low head position, urgently compensate for the circulating blood volume, the positive pressure at the end of mechanical ventilation is less than 10 cm when exhaling, and monitor the oxygen concentration. put in 100, with heart support ready when blood pressure drops severely.
Increased cerebral edema Need to deal with circulatory and respiratory problems:
Low blood pressure, blood theory . Ventilation: lack of oxygen The patient suddenly wakes up, feels pain At this time, the doctor should apply drugs that need Lasix, Mannitol or also a combination, Thiopental 1 to 2 mg/kg, analgesics, drugs Support muscle relaxation, put the patient into a high head position. Some surgeries are difficult to control cerebral edema because the brain already has severe swelling before surgery or the brain edema is suddenly at the same time when the skull is opened. What needs to be done urgently are: aspiration of the concentrated part of the brain tissue, removal of the brain lobe, removal of bones, and closure of the surgery.

3.3.4. Exit from anesthesia Severe trauma cases with GCS index less than 9 must be maintained sedated with mechanical ventilation immediately after surgery, at least the first 72 hours. Because at this time, cerebral edema is easy to progress to the most severe and life-threatening condition. 24 hours after surgery, the ventilator can be removed and the endotracheal tube is removed with the following conditions:
No respiratory phenomenon occurs and Circulatory system disorder before surgery GCS index immediately after surgery is not less than 9, no agitation occurred No increase in body weight and brain after surgery No associated trauma: maxillofacial trauma or trauma to the spine with paralysis or trauma to the chest and abdomen. Perform mechanical ventilation immediately after surgery for at least 3 hours for minor injuries, mechanical ventilation for 6 hours for moderate injuries without analgesia, sedation, or muscle relaxants. Once the endotracheal tube has been removed, the patient should be continuously monitored to avoid respiratory and circulatory disorders. Do not abuse pain relief during this time. It is necessary to reintubate the endotracheal tube as soon as the patient shows clinical signs of difficulty in breathing, exertion of breath, even though the SpO2 index has not decreased.
3.4. Postoperative resuscitation Reduce intracranial pressure Ensure good cerebral perfusion pressure. Fight any possible infection. Balance nutrition early for the body to recover
4. Risk of complications after anesthesia surgery traumatic brain injury
Risks and complications after surgical anesthesia are rare but not unheard of. It depends on your age, medical condition, type of anesthetic used and response to anesthesia.
4.1. Subjective factors Age: The older the person, the weaker the body's response to anesthesia, so it will be recognized more slowly after surgery than younger people. People who already have medical conditions such as diseases of the heart, vessels, nerves, smoking addiction, obesity ... the body reacts slowly to anesthetics, making the patient's body more tired. 4.2. Objective factors The procedure is simple or complicated: this affects the time of surgery, the longer the surgery, the longer the anesthesia must be maintained. Performing surgery in prepared conditions or in an emergency situation: the patient in an emergency is critical, the operation is urgent, many unusual complications occur requiring urgent medical attention. Timely response can lead to more dangerous complications. 4.3. Complications Local anesthesia There are usually few complications from local anesthesia. Overdose can cause poisoning when the anesthetic enters the body through the blood, affecting breathing, heart rate, blood pressure and other functions. Therefore, always have first aid equipment.
Endotracheal anesthesia Easier to occur. Anesthesia reduces oropharyngeal reflexes such as swallowing, coughing or spitting with the aim of avoiding aspiration into the lungs. Aspiration occurs when an object or liquid is inhaled into the airways (trachea or lungs). To prevent aspiration, people are intubated, patients are told not to eat or drink for a few hours before surgery to empty the stomach to avoid reflux of aspirated gastric juice into the lungs.
When placing or withdrawing the airway, the doctor often notices that the patient may have coughing, choking or muscle contractions in the larynx or trachea. Placing an airway can increase blood pressure, increase heart rate, break teeth, crush lips, laryngeal edema, sore throat, hoarseness caused by trauma, and laryngeal irritation.

Other risks of general anesthesia include:
Changes in blood pressure Changes in heart rate Heart attack Stroke Death or serious injury from injury: because anesthesia is rare and often associated with adverse events. evidence of surgery. Death can occur in about 1/250,000 cases with general anesthesia. Of course, the rate is higher for people with serious medical conditions, cases of severe allergies or shock, high fever, stroke or acute heart attack, aspiration pneumonia causing severe pneumonia, numbness. paralysis, pulmonary embolism or cerebral palsy.
Anesthesia does not completely cause loss of consciousness, but you may feel awake and aware during surgery. But in reality, awareness during anesthesia is rare as anesthesiologists often pay attention to avoid this and there are ways to prevent this from happening.
Secondary bleeding Secondary brain edema Incisional infection Epilepsy Seizure paralysis Anesthesia in traumatic brain injury surgery is an important step not to be subjective when conducting, usually the doctor will apply internal anesthesia trachea for brain surgery. Anesthesia ensures a smooth operation, avoids secondary injuries and maintains good resuscitation in the face of abnormal situations during surgery such as heavy blood loss, severe cerebral edema...
National General Hospital Vinmec hospital currently has a full range of modern medical equipment: Anesthesia machine, emergency resuscitation facilities, monitoring equipment: ultrasound machine, monitor, PCA, Auto bolus, nerve stimulator.. The hospital also has a team of doctors with many years of experience, well-trained in Anesthesia resuscitation / pain relief treatment, modern medical equipment to help monitor and take care of customers safely. . Therefore, when there are health problems, customers contact the hospital for advice and appropriate indications.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.