This is an automatically translated article.
Posted by Master, Doctor Dao Kim Phuong - Department of Examination - Vinmec Times City International Hospital1. Advanced cardiac assessment procedure
Fetal echocardiography provides a more detailed assessment of fetal cardiovascular structure and function than a baseline echocardiogram. A scientific statement from the American Heart Association states that a fetal echocardiogram should include standard images of the four chambers of the heart, the left and right ventricular outflow tracts, the three blood vessels, and the trachea. , aortic and pulmonary arches, superior and inferior vena cava, short axis and long axis, as well as color and pulse Doppler studies and pulse mode M to evaluate major veins, valves, and velocity , heart rate, etc. Guidelines for performing fetal echocardiography are also available from the International Society of Ultrasound in Obstetrics and Gynecology and from the American Institute of Medical Ultrasound.
The ultrasound system used for fetal echocardiography must be able to perform 2-D, M-mode, and Doppler imaging. Color Doppler and spectroscopy are used to identify small vessels such as the pulmonary veins, ductus venosus, and ductus arteriosus, to evaluate valve outflow, and to check for ventricular septal defects. The M-mode of atrial and ventricular wall motion can be useful for analyzing rhythm and rate disturbances.
More advanced imaging techniques include three- and four-dimensional echocardiography, tissue Doppler, strain and strain rate imaging, fetal electrocardiogram, fetal echocardiogram, and magnetic resonance imaging Heart.
Congenital heart disease (CHD) is associated with increased risk for adverse neurodevelopmental outcomes, thought to be due to factors such as associated chromosomal abnormalities, syndromes, cardiac dysfunction Postpartum, perioperative factors in the infant require surgical treatment and may be due to uterine hemodynamic abnormalities. In children with isolated cardiac abnormalities, the frequency of neurodevelopment also depends on the specific abnormality.
Prenatal neuroimaging findings are often not predictive of neurodevelopmental outcome after birth. A systematic review and meta-analysis of prenatal ultrasound and magnetic resonance imaging (MRI) studies found that brain abnormalities, head retardation, and encephalopathy were observed in the fetal segments. group of fetuses with CHD. However, the prognostic significance of these findings is unclear because large MRI studies are scarce, echocardiographic data favor severe left and left cardiac abnormalities, and long-term follow-up studies. relation to prenatal and postnatal findings is limited.

Fetal genetic evaluation is indicated because genetic abnormalities are common in fetuses with heart defects, even in isolation.
The risk of aneuploidy varies according to the anomaly. Example (percentage of risk):
Atrial septal defect, ventricular septal defect (46 - 73 %); And ductus arteriosus (19 - 78 %); Right ventricular malformation/double septal defect (6 - 43 %); Coarctation of the aorta/disruption of the aortic arch (5 - 37 %); Tricuspid valve dysplasia (including Ebstein anomaly, 4 - 16%); Tetralogy of Fallot (7 - 39 %); Hypoplastic left heart syndrome (HLHS, 4 - 9%); Right ventricular stenosis/hypoplasia with intact ventricular septum (1 - 12 %); Cardiac arrhythmia/arrhythmia syndrome (0%); Transposition of the great arteries (0 %); In addition, 22q11 deletion has been associated with several cardiac malformations, including interrupted aortic arch, common trunk, ventricular septal defect, and tetralogy of Fallot.
2. Follow up
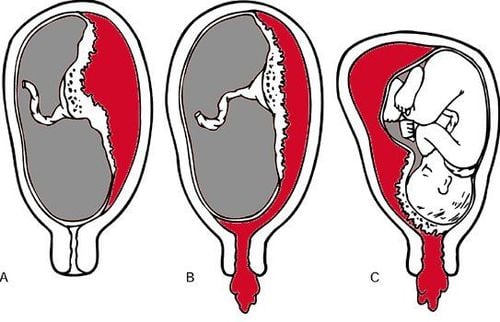
At least one follow-up visit early in the third trimester is reasonable to look for abnormalities that progress in severity or may not be detected earlier in pregnancy and are clinically significant postpartum . Some of the causes of progressive fetal cardiac dysfunction include worsening of valvular failure or obstruction, increased obstruction to blood flow in the great arteries, or development/worsening of the heart valve. myocarditis or cardiomyopathy, an arrhythmia, or a heart tumor.
An obstetrician will refer a pregnant patient to a pediatric cardiologist before delivery whenever fetal heart abnormalities are suspected on prenatal ultrasound. The purpose is to inform the patient of the suspected diagnosis and discuss pre- and postnatal management options, including the preferred location for delivery.
Transplacental drug therapy may improve the prognosis of some fetal arrhythmias.
Intrauterine invasive cardiac interventions (eg, aortic valve or balloon angioplasty, atrial septal defect dilation may improve the prognosis of some lesions, such as hypoplastic left heart HLHS or abnormal heart failure). Often severe valvular heart disease (eg, severe mitral regurgitation, coarctation of the aorta, pulmonary hypoplasia); however, these interventions are performed only at some fetal surgery centers.

3. During labor and delivery
Optimal care is required. Optimal care is defined as delivery of neonates with a prenatal diagnosis of critical congenital heart disease at or near a hospital with specialized neonatal cardiac care including balloon septal resection.
A birth plan should be planned in a facility with an appropriate level of care for the mother and the newborn. Neonates with ductal-dependent lesions, and most with severe cardiac damage, should be referred to a facility with expertise in grade III pediatric cardiology and the NICU. If this is not feasible, delivery should be arranged prior to delivery.
Cesarean section was performed according to standard obstetric indications, as there was no evidence that the fetal route of birth with congenital heart disease (CHD) influenced the outcome. Based on observational data, induction of labor or scheduled cesarean section before 39 weeks of gestation is not recommended in the absence of criteria for maternal or fetal concern regarding fetal health. infants, as even premature birth can lead to worse outcomes after cardiac surgery in infants. An exception may be single ventricular malformation, where earlier delivery may be beneficial.
Specialized delivery room care is recommended for fetuses with:
Type D transposition of the great arteries; Persistent or uncontrolled tachyarrhythmias with heart failure or fetal edema; Hypoplastic left heart syndrome (HLHS) with limited atrial septal defect or intact atrial septum and abnormal pulmonary venous outflow (pulmonary venous forward/reverse flow ratio <3) or hyperoxalemia abnormalities in the second trimester of pregnancy; Complete heart block and low ventricular rate, cardiac dysfunction or hydronephrosis. Care planning in a specialized delivery room may be considered for fetuses with:
Tetralogy of Fallot without a pulmonary valve; Ebstein anomaly with fetal edema; Return of the completely abnormal, obstructed pulmonary vein. There is no need for specialized delivery room care for these fetuses:
Mild tetralogy of Fallot, ventricular septal defect, atrial septal defect; Stream shunt; Most lesions are ductal dependent, but initiation of prostaglandin E1 may be indicated in the neonatal intensive care unit; Cardiac arrhythmias are controlled.

4. Summary and recommendations
Recommend prenatal screening for fetal heart abnormalities (Grade 2C). Prenatal diagnosis provides parents with the opportunity to gain prenatal prognostic information, learn about treatment options before and after birth, and make decisions regarding good management. best for their families and planning for specific birth needs. Depending on the lesion, prenatal diagnosis can reduce perinatal morbidity and mortality.
The optimal gestational age to screen for structural heart defects is 18 to 22 weeks' gestation. However, some fetal heart conditions may not be detected until, or may appear for the first time, after pregnancy. Fetal arrhythmias, myocarditis/myopathy, heart failure, valvular insufficiency or valvular obstruction, and cardiac tumors have different timing of onset. Atrial or ventricular septal defects, microvalvular lesions, partial anomalies of the pulmonary venous connection, and coronary artery anomalies are often not detected prior to surgery.
Increased risk of genetic abnormalities, especially aneuploidy or 22q11 deletion, in fetuses with CHD; The frequency of genetic abnormalities depends on the specific lesion. Current methods for genetic testing include (1) G-bands of fetal cells obtained through amniocentesis, with fluorescence in situ hybridization (FISH) for the evaluation of trace elements, such as such as 22q11, undetectable by visual banding and (2) chromosomal microscopy, which detects chromosomal abnormalities under the microscope in 5% of fetuses with anomalies detected by microscopy. Ultrasound and normal G-band karyotype. Either approach makes sense.
The need, timing, and frequency of follow-up echocardiography should be guided by the nature and severity of the lesion, the presence of heart failure, the predicted time and mechanism of progression, and Options are available for prenatal and postpartum interventions. We recommend at least one follow-up visit early in the third trimester to look for abnormalities that develop in severity or may go undetected earlier in pregnancy. For most lesions other than minor ventricular septal defects, we typically perform at least monthly examinations to assess disease progression and further counsel the patient.
The birth must be planned in a facility with an appropriate level of care for the mother and the newborn. Premature delivery and cesarean section are usually performed only for standard obstetric indications.
Risk assessment to anticipate harm in the delivery room or in the first few days postpartum is disease-specific.
Information has shown that prenatal diagnosis of critical congenital heart disease improves neonatal survival, further investigation is needed and efforts to improve prenatal diagnosis are needed congenital heart disease.
To protect the health of both mother and fetus, especially in the third trimester of pregnancy, which is the period of strong fetal development. Pregnant women need:
Comprehensive fetal malformation screening by superior 4D ultrasound technique. Screening for gestational diabetes, avoiding many dangerous complications for both mother and baby. Control the mother's weight reasonably to assess the health status of the pregnant woman and the development of the fetus. Understand the signs of threatened early delivery (especially in those carrying multiple pregnancies or having a history of miscarriage or premature birth) so that they can receive timely treatment to maintain pregnancy. To protect mother and baby during pregnancy, Vinmec provides a comprehensive Maternity service to monitor the health status of mother and baby, periodical antenatal check-ups with leading Obstetricians and Gynecologists. enough tests, important screening for pregnant women, counseling and timely intervention when detecting abnormalities in the health of mother and baby.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
REFERENCES
Holland BJ, Myers JA, Woods CR Jr. Prenatal diagnosis of critical congenital heart disease reduces risk of death from cardiovascular compromise prior to planned neonatal cardiac surgery: a meta-analysis. Ultrasound Obstet Gynecol 2015; 45:631.
Li YF, Zhou KY, Fang J, et al. Efficacy of prenatal diagnosis of major congenital heart disease on perinatal management and perioperative mortality: a meta-analysis. World J Pediatr 2016; 12:298.
Thakur V, Dutil N, Schwartz SM, Jaeggi E. Impact of prenatal diagnosis on the management and early outcome of critical duct-dependent cardiac lesions. Cardiol Young 2018; 28:548.
Khoshnood B, Lelong N, Houyel L, et al. Impact of prenatal diagnosis on survival of newborns with four congenital heart defects: a prospective, population-based cohort study in France (the EPICARD Study). BMJ Open 2017; 7:e018285.
Verheijen PM, Lisowski LA, Stoutenbeek P, et al. Prenatal diagnosis of congenital heart disease affects preoperative acidosis in the newborn patient. J Thorac Cardiovasc Surg 2001; 121:798.
Bonnet D, Coltri A, Butera G, et al. Detection of transposition of the great arteries in fetuses reduces neonatal morbidity and mortality. Circulation 1999; 99:916.
Freud LR, McElhinney DB, Marshall AC, et al. Fetal aortic valvuloplasty for evolving hypoplastic left heart syndrome: postnatal outcomes of the first 100 patients. Circulation 2014; 130:638.
Marshall AC, van der Velde ME, Tworetzky W, et al. Creation of an atrial septal defect in utero for fetuses with hypoplastic left heart syndrome and intact or highly restrictive atrial septum. Circulation 2004; 110:253.
Araujo Júnior E, Tonni G, Chung M, et al. Perinatal outcomes and intrauterine complications following fetal intervention for congenital heart disease: systematic review and meta-analysis of observational studies. Ultrasound Obstet Gynecol 2016; 48:426.
Friedman KG, Sleeper LA, Freud LR, et al. Improved technical success, postnatal outcome and refined predictors of outcome for fetal aortic valvuloplasty. Ultrasound Obstet Gynecol 2018; 52:212.
Committee on Practice Bulletins—Obstetrics and the American Institute of Ultrasound in Medicine. Practice Bulletin No. 175: Ultrasound in Pregnancy. Obstet Gynecol 2016; 128:e241.
http://www.aium.org/resources/guidelines/obstetric.pdf (Accessed on June 15, 2015).
Pinto NM, Nelson R, Puchalski M, et al. Cost-effectiveness of prenatal screening strategies for congenital heart disease. Ultrasound Obstet Gynecol 2014; 44:50.
Carvalho JS, Mavrides E, Shinebourne EA, et al. Improving the effectiveness of prenatal routine screening for major congenital heart defects. Heart 2002; 88:387.
Lloyd DFA, Pushparajah K, Simpson JM, et al. Three-dimensional visualization of the fetal heart using MRI with motion-corrected slice-volume registration: a prospective, single-center cohort study. Lancet 2019; 393:1619.
Jansen FA, Everwijn SM, Scheepjens R, et al. Fetal brain imaging in isolated congenital heart defects - a systematic review and meta-analysis. Prenat Diagn 2016; 36:601.
Copel JA, Cullen M, Green JJ, et al. The frequency of aneuploidy in prenatally diagnose congenital heart disease: an indication for fetal karyotyping. Am J Obstet Gynecol 1988; 158:409.
Wimalasundera RC, Gardiner HM. Congenital heart disease and aneuploidy. Prenat Diagn 2004; 24:1116.
Wallenstein MB, Harper LM, Odibo AO, et al. Fetal congenital heart disease and intrauterine growth restriction: a retrospective cohort study. J Matern Fetal Neonatal Med 2012; 25:662.
Perez-Delboy A, Simpson LL. Prenatal sonographic diagnosis of congenital heart disease and intrauterine growth restriction: a case-control study. J Clin Ultrasound 2007; 35:376.
Kipps AK, Feuille C, Azakie A, et al. Prenatal diagnosis of hypoplastic left heart syndrome in current era. Am J Cardiol 2011; 108:421.
Levey A, Glickstein JS, Kleinman CS, et al. The impact of prenatal diagnosis of complex congenital heart disease on neonatal outcomes. Pediatr Cardiol 2010; 31:587.
Atz AM, Travison TG, Williams IA, et al. Prenatal diagnosis and risk factors for preoperative death in neonates with single right ventricle and systemic outflow obstruction: screening data from the Pediatric Heart Network Single Ventricle Reconstruction Trial(∗). J Thorac Cardiovasc Surg 2010; 140:1245.