This is an automatically translated article.
Posted by Master, Doctor Dao Kim Phuong - Department of Examination - Vinmec Times City International Hospital
All cardiac lesions can be detected in the fetus based on timely fetal echocardiography, with the exception of a few minor lesions, such as atrial septal defects and ductus arteriosus. In some cases, prenatal diagnosis also offers the opportunity for in-utero treatment.
1. Make a problem
Newborn studies in Baltimore, Washington and studies in the US and UK have shown that a significant number of cases of congenital heart disease go undetected and lead to infant death. birth that was diagnosed only after an autopsy.
Existing studies have some limitations with respect to preoperative mortality assessment. There is a bias by excluding patients who died before heart surgery. Others are constrained by the small number of preoperative deaths or heterogeneous patient populations related to anatomic diagnosis, the presence of risk factors, and the family's desire to pursue surgery. heart surgery. Most studies to date have not allowed accurate comparisons between groups due to lack of detailed information on cardiac anatomy or preoperative causes of death.
This analysis shows that prenatal diagnosis of critical congenital heart disease improves neonatal survival. Infants diagnosed postpartum are more likely to die from cardiovascular damage before planned heart surgery than those diagnosed before birth.
Prenatal identification and management of fetal heart abnormalities is important because birth defects are the leading cause of infant mortality and congenital heart disease accounts for 30 to 50% of cases. this fatality. In general, all cardiac lesions can be detected in the fetus based on timed fetal echocardiography, with the exception of some minor lesions, such as second foraminal septal defects and ductus arteriosus. Atrial septal defect and ductus arteriosus are normal fetal shunts.
Prenatal diagnosis of heart disease offers parents the opportunity to gain prenatal prognostic information, learn about treatment options before and after birth, make decisions regarding management the best management for their family (eg, abortion or undergoing intrauterine intervention, if available; no intervention), and planning for specific birth needs (eg, place of birth, home provides pediatric and obstetric services, delivery, and palliative care). It may also improve neonatal outcomes. Because of the complexity of these issues, referral to a maternal-fetal specialist, pediatric cardiologist, geneticist, and/or neonatologist is recommended.
Prenatal diagnosis of heart disease has also been associated with a reduced incidence of neonatal morbidity, including severe acidosis. Newborns with congenital heart defects that require ductal support for systemic or pulmonary circulation may benefit from early postpartum intervention (prostaglandin E1) to prevent ductal closure. Similarly, readiness to perform transluminal intervention (eg, balloon atrial septal defect resection for patients with type D major artery transposition [TGA] or hypoplastic left heart syndrome [HLHS], angioplasty) balloon valve for patients with critical pulmonary or aortic stenosis) or pacing immediately after birth helps to rapidly stabilize the postpartum circulation and thus may improve outcomes.

In some cases, prenatal diagnosis also offers the opportunity for in-utero treatment. Transplacental drug therapy improves the prognosis of some fetal arrhythmias, especially tachycardia. Intrauterine invasive cardiac intervention (eg, aortic or balloon angioplasty, atrial septal defect dilation) may improve prognosis for some lesions, such as HLHS or severe valvular abnormalities. eg, severe aortic stenosis, pulmonary hypoplasia); however, these interventions are only performed at some fetal surgery centers.
2. Screening time
The optimal gestational age for screening for structural heart defects is between 18 and 22 weeks. Fetal cardiac anatomy can be well visualized at this stage of pregnancy, and further evaluation (eg, echocardiography, chromosomal) can be performed, if indicated, while the fetus is still alive. .
After 30 weeks of gestation, it can be difficult to obtain an optimal image as the fetus becomes more and more cramped in the amniotic cavity. It should be noted that some fetal heart conditions may not be detected until or may appear for the first time after 18 to 22 weeks of gestation. For example, fetal arrhythmias, myocarditis/myopathy, heart failure, valvular insufficiency or obstruction, and cardiac tumors have variable onset times.
In addition, small atrial or ventricular septal defects, mild valvular lesions, partial pulmonary venous connection abnormalities, and coronary artery anomalies are often not detected in pregnancy.
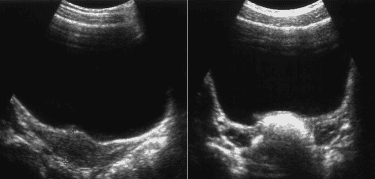
3. Standard Cardiovascular Assessment
There is a large variation in detection rates between screening studies, with some studies reporting only 15% detection of congenital heart disease (CHD). Factors that influence sensitivity include type of ultrasound practice (eg, university versus community hospital), operator training and experience, gestational age, maternal weight, position fetal intelligence and type of disability. Fetal echocardiography is a more sensitive but less cost-effective screening method for low-risk pregnancies for CHD.
4. Advanced Cardiovascular Assessment
Advanced fetal echocardiography should be performed in fetuses at high risk of congenital heart disease (CHD).
American Heart Association (AHA), American Society of Echocardiography (ASE), and Society of Pediatric and Congenital Electrophysiology (PACES) recommend fetal echocardiography in cases of:
Pregnant women with gestational diabetes or diabetes diagnosed in the first 3 months; Phenylketonuria in the mother (uncontrolled); Maternal autoimmune disease, maternal autoantibodies (SSA/SSB), especially if the child has previously had SSA/SSB-related heart disease; Maternal teratogens when administered with drugs (eg, thalidomide, ACE inhibitors, retinoic acid, nonsteroidal anti-inflammatory drugs [NSAIDs] during the third trimester); Maternal rubella infection during the first 3 months of pregnancy; Maternal infection with suspected fetal myocarditis because of poor contractility or effusion on standard 4-chamber cardiac examination (eg, coxsackie virus, adenovirus, cytomegalovirus); Pregnancy using assisted reproductive technology (ART); Congenital heart in a first-degree relative of the fetus (mother, father or sibling); First- or second-degree relatives associated with congenital heart-linked Mendelian disorders (eg, Noonan, tuberous sclerosis, Holt-Oram, DiGeorge syndrome/22q11 deletion, syndrome Alagille, Williams syndrome);

Suspected fetal heart abnormalities (structure, function, arrhythmia) on obstetric ultrasound; Suspected fetal heart abnormalities on obstetric ultrasound; Fetal chromosomal testing showing genetic mutation, deletion, rearrangement or aneuploidy; Fast or slow fetal heart rate or irregular or persistent heartbeat; Fetal nuchal translucency increased > 95 percent (≥3mm) on first-trimester ultrasound; Twins with the same egg; Effusion or edema. To protect the health of both mother and fetus, especially in the third trimester of pregnancy, which is the period of strong fetal development. Pregnant women need:
Comprehensive fetal malformation screening by superior 4D ultrasound technique. Screening for gestational diabetes, avoiding many dangerous complications for both mother and baby. Control the mother's weight reasonably to assess the health status of the pregnant woman and the development of the fetus. Understand the signs of threatened early delivery (especially in those carrying multiple pregnancies or having a history of miscarriage or premature birth) so that they can receive timely treatment to maintain pregnancy. To protect mother and baby during pregnancy, Vinmec provides a comprehensive Maternity service to monitor the health status of mother and baby, periodical antenatal check-ups with leading Obstetricians and Gynecologists. enough tests, important screening for pregnant women, counseling and timely intervention when detecting abnormalities in the health of mother and baby.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
REFERENCES
Holland BJ, Myers JA, Woods CR Jr. Prenatal diagnosis of critical congenital heart disease reduces risk of death from cardiovascular compromise prior to planned neonatal cardiac surgery: a meta-analysis. Ultrasound Obstet Gynecol 2015; 45:631.
Li YF, Zhou KY, Fang J, et al. Efficacy of prenatal diagnosis of major congenital heart disease on perinatal management and perioperative mortality: a meta-analysis. World J Pediatr 2016; 12:298.
Thakur V, Dutil N, Schwartz SM, Jaeggi E. Impact of prenatal diagnosis on the management and early outcome of critical duct-dependent cardiac lesions. Cardiol Young 2018; 28:548.
Khoshnood B, Lelong N, Houyel L, et al. Impact of prenatal diagnosis on survival of newborns with four congenital heart defects: a prospective, population-based cohort study in France (the EPICARD Study). BMJ Open 2017; 7:e018285.
Verheijen PM, Lisowski LA, Stoutenbeek P, et al. Prenatal diagnosis of congenital heart disease affects preoperative acidosis in the newborn patient. J Thorac Cardiovasc Surg 2001; 121:798.
Bonnet D, Coltri A, Butera G, et al. Detection of transposition of the great arteries in fetuses reduces neonatal morbidity and mortality. Circulation 1999; 99:916.
Freud LR, McElhinney DB, Marshall AC, et al. Fetal aortic valvuloplasty for evolving hypoplastic left heart syndrome: postnatal outcomes of the first 100 patients. Circulation 2014; 130:638.
Marshall AC, van der Velde ME, Tworetzky W, et al. Creation of an atrial septal defect in utero for fetuses with hypoplastic left heart syndrome and intact or highly restrictive atrial septum. Circulation 2004; 110:253.
Araujo Júnior E, Tonni G, Chung M, et al. Perinatal outcomes and intrauterine complications following fetal intervention for congenital heart disease: systematic review and meta-analysis of observational studies. Ultrasound Obstet Gynecol 2016; 48:426.
Friedman KG, Sleeper LA, Freud LR, et al. Improved technical success, postnatal outcome and refined predictors of outcome for fetal aortic valvuloplasty. Ultrasound Obstet Gynecol 2018; 52:212.
Committee on Practice Bulletins—Obstetrics and the American Institute of Ultrasound in Medicine. Practice Bulletin No. 175: Ultrasound in Pregnancy. Obstet Gynecol 2016; 128:e241.
http://www.aium.org/resources/guidelines/obstetric.pdf (Accessed on June 15, 2015).
Pinto NM, Nelson R, Puchalski M, et al. Cost-effectiveness of prenatal screening strategies for congenital heart disease. Ultrasound Obstet Gynecol 2014; 44:50.
Carvalho JS, Mavrides E, Shinebourne EA, et al. Improving the effectiveness of prenatal routine screening for major congenital heart defects. Heart 2002; 88:387.
Lloyd DFA, Pushparajah K, Simpson JM, et al. Three-dimensional visualization of the fetal heart using MRI with motion-corrected slice-volume registration: a prospective, single-center cohort study. Lancet 2019; 393:1619.
Jansen FA, Everwijn SM, Scheepjens R, et al. Fetal brain imaging in isolated congenital heart defects - a systematic review and meta-analysis. Prenat Diagn 2016; 36:601.
Copel JA, Cullen M, Green JJ, et al. The frequency of aneuploidy in prenatally diagnose congenital heart disease: an indication for fetal karyotyping. Am J Obstet Gynecol 1988; 158:409.
Wimalasundera RC, Gardiner HM. Congenital heart disease and aneuploidy. Prenat Diagn 2004; 24:1116.
Wallenstein MB, Harper LM, Odibo AO, et al. Fetal congenital heart disease and intrauterine growth restriction: a retrospective cohort study. J Matern Fetal Neonatal Med 2012; 25:662.
Perez-Delboy A, Simpson LL. Prenatal sonographic diagnosis of congenital heart disease and intrauterine growth restriction: a case-control study. J Clin Ultrasound 2007; 35:376.
Kipps AK, Feuille C, Azakie A, et al. Prenatal diagnosis of hypoplastic left heart syndrome in current era. Am J Cardiol 2011; 108:421.
Levey A, Glickstein JS, Kleinman CS, et al. The impact of prenatal diagnosis of complex congenital heart disease on neonatal outcomes. Pediatr Cardiol 2010; 31:587.
Atz AM, Travison TG, Williams IA, et al. Prenatal diagnosis and risk factors for preoperative death in neonates with single right ventricle and systemic outflow obstruction: screening data from the Pediatric Heart Network Single Ventricle Reconstruction Trial(∗). J Thorac Cardiovasc Surg 2010; 140:1245.